Lymphoma is the most common of heterogeneous malignant tumors caused by malignant transformation of lymphocytes. Such tumors usually originate from the lymph nodes or other lymphatic tissues. From the 1970s to the 1990s, the prevalence of lymphoma in the United States increased at an annual rate of 3%-4%. With the aggravation of environmental pollution, the incidence of lymphoma is getting higher and higher, and it is showing a younger trend. Lymphoma mainly includes two types, Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL). And non-Hodgkin lymphoma is much more common than Hodgkin lymphoma. In this article, we primarily focus on non-Hodgkin lymphoma, including key points of this disease as follows:
1. What is Non-Hodgkin's Lymphoma?
Non-Hodgkin's lymphoma (NHL) is cancer that originates in your lymphatic system, the disease-fighting network spread throughout your body. In NHL, tumors develop from lymphocytes — a type of white blood cell. NHL most often affects adults, but children can get it too. NHL is one of the most common cancers in the United States, accounting for about 4% of all cancers. In 2020, the American Cancer Society's estimates that there are about 77,240 people (42,380 males and 34,860 females) diagnosed with NHL, and about 19,940 people died from this cancer (11,460 males and 8,480 females).
Overall, the chance that a man will develop NHL in his lifetime is about 1 in 41; for a woman, the risk is about 1 in 52. Additionally, U.S. surveillance epidemiology and end results (SEER) incidence data show that men are more likely to develop NHL than women, and lymphomas are most common in white people, followed by black, yellow and brown people [1]. In the United States from 2000 to 2003, the average age of patients diagnosed with NHL was 67 years old, less than 2% of patients were younger than 20 years old, 47% of patients were between 65 and 84 years old, and 8% of patients were older than 84 years old.
2. What Are the Types of Non-Hodgkin's Lymphoma?
The type of lymphoma depends on what type of lymphocyte is affected (B cells or T cells), how mature the cells are when they become cancerous, and other factors. The lymph system is made up mainly of lymphocytes, a type of white blood cell that helps the body fight infections, including B lymphocytes (B cells) and T lymphocytes (T cells).
Lymphoma can start in either type of lymphocytes, but B-cell lymphomas are most common. The American Cancer Society estimates that 85% NHL cases are B-cell lymphomas. Among of them, the most common types of B-cell lymphomas are diffuse large B-cell lymphoma (DLBCL), which accounts for 1 out of every 3 cases in the United States and follicular lymphoma, which accounts for 1 out of every 5 cases in the United States.
Based on how fast they grow and spread, NHL can be divided into indolent lymphomas and aggressive lymphomas. Indolent lymphomas grow and spread slowly, and some indolent lymphomas just need to be watched closely instead of being treated right away. The most common type of indolent lymphoma in the United States is follicular lymphoma. Aggressive lymphomas grow and spread quickly, and usually need to be treated right away. The most common type of aggressive lymphoma in the United States is diffuse large B cell lymphoma (DLBCL).
3. What is the Pathogenesis of Non-Hodgkin's Lymphoma?
As mentioned before, most NHLs start in B cell. In this section, we mainly pay attention to the pathogenesis of NHL caused by abnormal B cells. Generally, B cell development is initiated in the primary lymphoid organs with subsequent differentiation in secondary lymphoid tissues such as lymph nodes, spleen, or tonsils. During these different steps of B cell differentiation, recurrent translocations occur that are often an initial step in the malignant transformation. These accumulation of genetic aberrations induce a selective growth advantage of the malignant clone leading to lymphoma evolution.
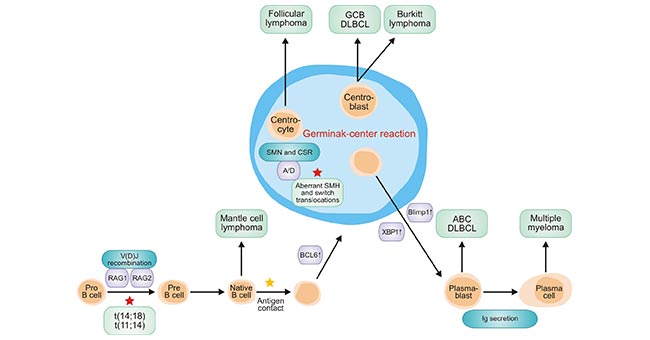
Figure 1. Lymphomas arise at different stages of B-cell differentiation
*this diagram is derived from publication on JOURNAL OF CLINICAL ONCOLOGY [2].
As the figure 1 shows, several specific recombination events are prone to the development of chromosomal aberrations. Recombination activating gene 1 (RAG1)-dependent and RAG2-dependent V(D)J recombination occur in the bone marrow. The potentially resulting t (14;18) and t (11;14) represent critical first steps in lymphomagenesis of different lymphoma subtypes [3] [4].
After antigen contact, the stimulated B cells transfer to the lymph node and form the germinal center after upregulation of BCL6. The events during the germinal center reaction include somatic hypermutation (SHM) and class-switch recombination (CSR). Both of them are mediated by the B-cell activation-induced cytidine deaminase (AID) [5] and are critical events for lymphoma evolution. The germinal center reaction is terminated by the differentiation of B cells into plasma cells. XBP1 and Blimp-1 are key regulators for plasmacytic differentiation.
4. What Causes Non-Hodgkin Lymphoma?
In fact, the exact cause of non-Hodgkin lymphoma is still unknown. It occurs when the body makes too many abnormal lymphocytes. These abnormal cells don't die and continue to grow and divide. This enlarges the lymph nodes. Currently, there are multiple medical conditions that are associated with an increased risk of developing the disease, including inherited immune deficiencies, genetic syndromes (Down syndrome and Klinefelter's syndrome), immune disorders, and their treatments (Sjögren's syndrome, rheumatoid arthritis, systemic lupus erythematosus), celiac disease, inflammatory bowel disease (particularly Crohn's disease), psoriasis and family history of lymphoma.
Moreover, several bacteria and viruses also can increase the risk of developing non-Hodgkin Lymphoma. Bacteria include helicobacter pylori (associated with gastritis and gastric ulcers), borrelia burgdorferi (associated with Lyme disease), campylobacter jejuni and chalmydia psittaci. And viruses usually involve HIV, HTLV-1, SV-40, HHV-8, Epstein Barr virus and hepatitis virus.
Note:
Klinefelter's syndrome is a genetic condition in men caused by an extra X chromosome. Sjögren's syndrome is an immune disorder characterized by unusual dryness of mucous membranes. Celiac disease refers to a disease involving the processing of certain components of gluten, a protein in grains
Additionally, chemicals, such as those used to kill insects and weeds, may increase your risk of developing non-Hodgkin's lymphoma. Older age also is a risk factor of getting non-Hodgkin's lymphoma. Although non-Hodgkin's lymphoma can occur at any age, but the risk increases with age. It's most common in people 60 or over.
5. What's the difference between Hodgkin and non-Hodgkin lymphoma?
As mentioned previously, lymphoma can be divided into two types, including Hodgkin and non-Hodgkin's lymphoma. They may sound very similar, but they are also two very different types of cancers. The differences in these two types of lymphoma are certain unique characteristics of the different lymphoma cells. They can be distinguished by using a microscope to look for Reed-Sternberg cells. Reed-Sternberg cells are a type of cell that appears in people with Hodgkin disease, or Hodgkin lymphoma. The number of these Reed-Sternberg cells increase as the disease advances. But non-Hodgkin's lymphoma does not contain Reed-Sternberg cells.
Furthermore, the age of getting disease in the two types of lymphoma is different. The average age of someone who is diagnosed with non-Hodgkin's lymphoma is 60, while most Hodgkin lymphomas occur in people ages 15 to 24, or over 60. Though the symptoms of Hodgkin and non-Hodgkin's lymphoma can be difficult to detect, both symptoms include painless swelling of lymph nodes that can be found anywhere on your body. Hodgkin's lymphoma is more likely to begin in lymph nodes in your upper body, such as your neck, underarms and chest.
Regarding to prognosis, hodgkin lymphoma is considered one of the most treatable cancers, with more than 90 percent of patients surviving more than five years.
References
[1] Susan G Fisher and Richard I Fisher. The epidemiology of non-Hodgkin's lymphoma [J]. Oncogene. 2004, 23, 6524–6534.
[2] Hendrik Nogai, Bernd Do¨rken, and Georg Lenz. Pathogenesis of Non-Hodgkin's Lymphoma [J]. JOURNAL OF CLINICAL ONCOLOGY. 2011, 29 (14): 1803-1811.
[3] Fugmann SD, Lee AI, Shockett PE, et al. The RAG proteins and V(D)J recombination: Complexes, ends, and transposition [J]. Annu Rev Immunol. 2000, 18:495-527.
[4] Rajewsky K. Clonal selection and learning in the antibody system [J]. Nature. 1996, 381:751-758.
[5] Muramatsu M, Kinoshita K, Fagarasan S, et al. Class switch recombination and hypermutation require activation-induced cytidine deaminase (AID), a potential RNA editing enzyme [J]. Cell. 2000, 102:553-563.
CUSABIO team. Non-Hodgkin's Lymphoma, One of Common Heterogeneous Malignant Tumors. https://www.cusabio.com/c-21009.html




Comments
Leave a Comment