Endometrial cancer, a prevalent gynecological malignancy in women, has witnessed a rising incidence in recent years, garnering global medical attention. With evolving lifestyle and environmental factors, the pathogenesis of endometrial cancer has become increasingly intricate. A profound understanding of the biological characteristics of endometrial cancer is paramount for formulating effective treatment strategies, improving patient survival rates, and enhancing overall quality of life. This article aims to provide you with comprehensive information on the biology of endometrial cancer, encompassing its anatomy and physiology, etiology and risk factors, molecular biology, pathology, immunotherapy, molecular markers, and more. By delving into the biological complexity of endometrial cancer, we can better comprehend its pathogenic mechanisms, laying the foundation for future advancements in treatment and prevention.
1. Anatomy and Physiology of the Endometrium
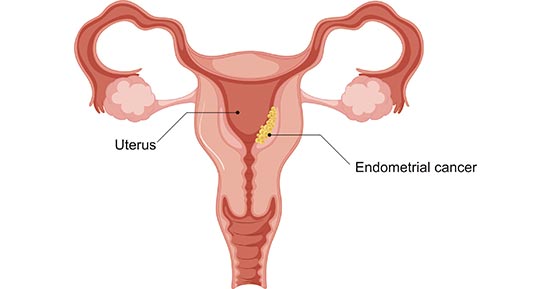
The endometrium constitutes the innermost layer of the uterine cavity, featuring a complex and finely tuned structure with physiological functions. Understanding the normal functioning of the endometrium under physiological conditions is crucial for unraveling the pathogenic mechanisms of endometrial cancer.
Figure 1. a diagram of endometrial cancer
1.1 Structure and Function
The endometrium is composed of multiple layers of epithelial cells, glands, and connective tissue. These structures undergo dynamic changes throughout the reproductive cycle of females. At different stages of the menstrual cycle, the endometrium undergoes alterations, including proliferation, differentiation, and shedding, to provide an optimal environment for potential fertilization. Key components include glandular cells, basal cells, and stromal cells, working in coordination to maintain a normal physiological state.
1.2 Changes in the Menstrual Cycle
The menstrual cycle consists of the menstrual phase, follicular phase, ovulatory phase, and luteal phase. In the early stages of the menstrual cycle, the endometrium undergoes thickening and glandular proliferation to prepare for potential pregnancy. If fertilization does not occur, the endometrium undergoes shedding, resulting in menstrual flow. This cyclical change is regulated by fluctuations in hormone levels, including estrogen and progesterone.
1.3 Relation to Endometrial Cancer
Endometrial cancer typically originates from the epithelial cells of the endometrium, where abnormal regulation of hormones and disruptions in cell growth signals may be key factors leading to carcinogenesis. Understanding the physiological changes in the endometrium under normal circumstances helps identify abnormal processes associated with cancer development.
In-depth exploration of the anatomy and physiology of the endometrium provides a foundation for understanding the origin and development of endometrial cancer, offering crucial background knowledge for subsequent sections on etiology and molecular mechanisms.
2. Causes and Risk Factors of Endometrial Cancer
The onset of endometrial cancer involves various factors, primarily including hormonal imbalance, obesity, genetic factors, and family history.
- Hormonal Imbalance: Elevated estrogen levels, especially hormonal irregularities associated with early menstruation, late childbirth, infertility, and related factors, are major risk factors for endometrial cancer.
- Obesity: Obesity is an independent risk factor for endometrial cancer. Excessive adipose tissue leads to an increase in estrogen levels in the body, prompting abnormal proliferation of the endometrium.
- Genetic Factors and Family History: Specific genetic mutations, such as those associated with Lynch syndrome, are linked to an increased risk of endometrial cancer. Having cases of endometrial cancer in the family also raises an individual's risk of developing the disease.
In-depth research into these factors contributes to a comprehensive understanding of the mechanisms behind endometrial cancer development, laying the foundation for the formulation of personalized prevention and treatment strategies.
3. Molecular Biology of Endometrial Cancer
Research into the molecular biology of endometrial cancer has unveiled changes at multiple levels, including gene mutations, abnormalities in DNA repair mechanisms, and inactivation of tumor suppressor genes, profoundly influencing cancer development and progression.
3.1 Gene Mutations
The onset of endometrial cancer is closely associated with mutations in multiple genes. The mutation of the TP53 gene is particularly significant, leading to the loss of normal growth regulatory mechanisms in cells. Other common gene mutations include KRAS, PTEN, among others, collectively contributing to uncontrolled proliferation of cancer cells.
3.2 DNA Repair Mechanisms
Aberrant DNA repair mechanisms play a crucial role in the development of endometrial cancer. Abnormal expression or loss of DNA repair-related genes results in genomic instability, providing a foundation for the evolution of cancer cells. Mutations in genes such as BRCA1 and BRCA2 are closely linked to abnormalities in DNA repair mechanisms and are key factors in the genetic susceptibility to endometrial cancer.
3.3 Tumor Suppressor Genes
The abnormal expression of multiple tumor suppressor genes is associated with the onset of endometrial cancer. The loss of the PTEN gene is closely linked to the activation of the PI3K/Akt signaling pathway, prompting cancer cells to evade normal apoptotic mechanisms and achieve uncontrolled growth.
3.4 Signaling Pathways
The development of endometrial cancer is intricately regulated by multiple signaling pathways. The abnormal activation of the PI3K/Akt signaling pathway directly participates in the regulation of cell survival and proliferation, creating favorable conditions for cancer cell survival. The abnormal activation of the Wnt/β-catenin signaling pathway is associated with the loss of cell polarity and uncontrolled proliferation. The inactivation of the p53 pathway impacts the regulation of the cell cycle and apoptotic mechanisms, providing favorable conditions for cancer cell evasion.
A profound understanding of these molecular biological changes not only aids in comprehending the mechanisms behind the onset of endometrial cancer but also provides a theoretical foundation for the development of more precise molecular targeted therapies.
4. Pathology of Endometrial Cancer
The pathology research of endometrial cancer encompasses various aspects, from the morphological characteristics of the tumor to the staging of its clinical manifestations. The following is a detailed exploration of the pathology of endometrial cancer:
4.1 Tumor Types
Endometrioid Adenocarcinoma: This is the most common type of endometrial cancer, accounting for approximately 80% of all cases. Its characteristic feature is the formation of glandular structures by cancer cells, usually presenting in a well-differentiated state.
Invasive Papillary Serous Carcinoma: Relatively rare but often exhibiting high invasiveness. Cancer cells in this type form papillary structures with disordered cell arrangements.
4.2 Tumor Grade
The tumor grade of endometrial cancer is directly related to the similarity of its cells. The degree of differentiation is categorized into high, moderate, and low grades. Highly differentiated cancer cells typically resemble normal cells more closely, while low differentiation implies greater heterogeneity.
4.3 Staging
Early Stage (I, II): Cancer is confined to the endometrium or invades the uterine muscle layer, without spreading to other organs.
Intermediate Stage (III): Cancer cells spread to nearby tissues and lymph nodes but have not involved distant organs.
Advanced Stage (IV): Cancer cells spread to distant organs such as the bladder, rectum, or distant lymph nodes.
4.4 Other Pathological Features
Vascular Invasion: Some endometrial cancers show invasion into blood vessels, which may increase the risk of cancer cell spread.
Infiltrative Growth: In some cases, cancer cells exhibit infiltrative growth, meaning they invade surrounding normal tissues.
The pathological characteristics of endometrial cancer are crucial for determining treatment plans and prognosis. Understanding tumor types, differentiation grades, and staging helps physicians develop personalized treatment strategies, enhancing treatment effectiveness.
5. Molecular Biomarkers of Endometrial Cancer
Molecular biomarkers play a crucial role in the early diagnosis, treatment selection, and prognosis assessment of endometrial cancer. Here are some key molecular biomarkers associated with endometrial cancer:
- Microsatellite Instability (MSI): MSI is a marker associated with DNA repair instability and is closely linked to the occurrence and development of endometrial cancer. Detecting MSI can help determine the genetic characteristics of the tumor, guide treatment, and assess patient prognosis.
- DNA Methylation Biomarkers: Changes in DNA methylation, including high methylation in gene promoter regions, are present in endometrial cancer. These methylation biomarkers can be used to differentiate subtypes of endometrial cancer, providing more precise diagnostic information.
- Mismatch Repair Deficiency (DNA Mismatch Repair Deficiency): Defects in the DNA mismatch repair system are relatively common in endometrial cancer. Detecting mismatch repair deficiency can help determine whether patients are suitable for specific immunotherapies, such as PD-1/PD-L1 inhibitors.
- PTEN Gene: PTEN is a critical gene that inhibits cell growth and differentiation, and its mutation or loss is associated with the occurrence of endometrial cancer. Testing the status of the PTEN gene helps assess the biological characteristics of the tumor and its sensitivity to treatment.
- p53 Protein: p53 is an important tumor suppressor protein, and its abnormal expression in endometrial cancer is correlated with tumor invasiveness and prognosis. Determining the expression levels of the p53 protein helps understand the malignancy of the tumor.
In-depth research into these molecular biomarkers contributes to a better understanding of the molecular mechanisms of endometrial cancer, providing a basis for precision medicine and personalized treatment. The detection of these biomarkers assists doctors in more accurately formulating treatment plans, thereby improving patient survival rates and quality of life.
6. Latest Research Advances
Endometrial cancer is one of the most common gynecological cancers in developed countries, and its incidence has been steadily increasing over the years, making it one of the leading causes of cancer-related deaths in the United States. The following highlights the latest research advances in endometrial cancer:
Importance of Estrogen Signaling Pathway: Rodriguez et al.emphasize the significance of the estrogen signaling pathway in endometrial cancer. They provide a detailed discussion of the specific role of estrogen receptors (ER) in endometrial cancer and pose open questions regarding estrogen signaling in this cancer[1].
Clinical Applications of Molecular Features: Urick et al. stress the potential clinical utility of molecular features in early detection, risk stratification, and guiding targeted therapies for endometrial cancer. This opens new directions for the development of personalized treatment approaches[2].
Risk Assessment of Endometrial Hyperplasia and Carcinogenesis: Doherty et al. point out the need for quantifying the potential for concurrent endometrial cancer and the future risk of progression to cancer in patients with endometrial hyperplasia to inform treatment decisions. This holds guiding significance for personalized treatment[3].
Genetic Mutations and Immunotherapy: Deshpande et al. mention the association of Lynch syndrome with endometrial cancer and introduce a novel immunotherapy for treating solid tumors with microsatellite instability (MSI)[4].
Advancements in Treatment Strategies: Makker et al. summarize the latest understanding of endometrial cancer epidemiology, pathophysiology, diagnosis, molecular classification, and recent advancements in disease management. They emphasize the diversity of treatment strategies aiming to improve precision in treating this complex malignancy[5].
Driving Forces of Molecular Biology: Crosbie et al. highlight that a deeper understanding of the molecular biology of endometrial cancer paves the way for the development of targeted therapeutic strategies. Clinical trials are expected to demonstrate their benefits in adjuvant, advanced, and recurrent cases in the coming years[6].
These recent research advances provide crucial information for better understanding, preventing, and treating endometrial cancer, presenting challenges and opportunities for future clinical practice and research efforts.
References
[1] Adriana C Rodriguez, Zannel Blanchard, Kathryn A Maurer, Jason Gertz, "Estrogen Signaling in Endometrial Cancer: A Key Oncogenic Pathway with Several Open Questions", HORMONES & CANCER, 2019.
[2] Mary Ellen Urick, Daphne W Bell, "Clinical Actionability of Molecular Targets in Endometrial Cancer", NATURE REVIEWS. CANCER, 2019.
[3] Michelle T Doherty, Omolara B Sanni, Helen G Coleman, et al. "Concurrent and Future Risk of Endometrial Cancer in Women with Endometrial Hyperplasia: A Systematic Review and Meta-analysis", PLOS ONE, 2020.
[4] Madhura Deshpande, Phillip A Romanski, Zev Rosenwaks, Jeannine Gerhardt, "Gynecological Cancers Caused By Deficient Mismatch Repair and Microsatellite Instability", CANCERS, 2020.
[5] Angela K Green, Jacqueline Feinberg, Vicky Makker, "A Review Of Immune Checkpoint Blockade Therapy In Endometrial Cancer", AMERICAN SOCIETY OF CLINICAL ONCOLOGY EDUCATIONAL BOOK. ..., 2020.
[6] Emma J Crosbie, Sarah J Kitson, Jessica N McAlpine, et al. "Endometrial Cancer", LANCET (LONDON, ENGLAND), 2021.
CUSABIO team. Decoding the Biological Complexity of Endometrial Cancer: Essential Insights for Researchers. https://www.cusabio.com/c-21001.html




Comments
Leave a Comment