Our immune system keeps us from disease, killing bacteria and viruses. T cell is one main type of immune cell. Proteins on the surface of T cells, called immune checkpoints, aim to turn on an immune response or turn it off. Some immune checkpoint proteins help tell T cells to become active, for example when an infection is present. But if T cells are active for too long, or react to things they shouldn't, they can start to destroy healthy cells and tissues. So other immune checkpoints help tell T cells to switch off. Some cancer cells make high levels of proteins. These can switch off T cells, when they should really be attacking the cancer cells. So the cancer cells are pushing a stop button on the immune system. And the T cells can no longer recognize and kill cancer cells.
An immune checkpoint inhibitor, one type of immune checkpoint drugs, is used to block immune checkpoint proteins. They stop the proteins on the cancer cells from pushing the stop button. This turns the immune system back on and the T cells are able to find and attack the cancer cells.
Three checkpoint inhibitors have received rapid approval from the U.S. Food and Drug Administration for cancer, including ipilimumab (Yervoy®), pembrolizumab (Keytruda®), and nivolumab (Opdivo®). These and other immune checkpoint therapies represent one of the most promising frontiers in cancer treatment today. Here we numerate two kinds of typical checkpoint inhibitors and introduce their related mechanism briefly.
Yervoy®- ipilimumab (CTLA-4 Antibody)
CTLA-4, also known as CD152, is a transmembrane protein encoded by the CTLA-4 gene expressed in activated CD4+ and CD8+ T cells with high homology to the co-stimulatory molecule receptor (CD28) on the surface of T cells. Both CTLA-4 and CD28 are members of the immunoglobulin superfamily, which bind to the same ligands CD86 (B7-2) and CD80 (B7-1). The key to the immunoregulatory function of CTLA-4 is the control of CD4+, CD8+ T cells, and regulatory T cells (Treg). CTLA-4 is able to prevent the T cell response of activated cells and mediate the inhibitory function of Treg.
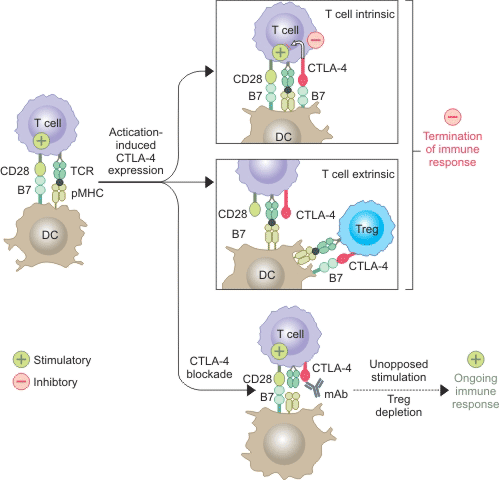
Current studies indicate that CTLA-4 inhibits T cell responses mainly through two pathways (Figure 1). One is to reduce B7 by competitive binding to CD28 or to recruit phosphatase to the intracellular domain of CTLA-4. The other is to reduce the expression levels of CD80 and CD86 in antigen presenting cells (APC) or to remove them from APC by transendocytosis, thus reducing CD28 involvement in T cell activation. In addition, CTLA-4 also mediates dendritic cell binding to CD80/CD86 and induces expression of the tryptophan degrading enzyme IDO, resulting in inhibition of TCR. The CTLA-4 antibody reduces Treg by binding to CTLA-4 and activates TCR.
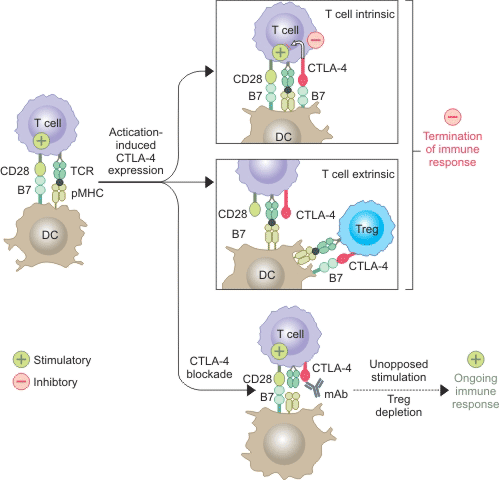
Figure 1. CTLA-4 inhibits T cell responses mainly through two pathways
Keytruda®- pembrolizumab (PD-1 antibody)
PD-1, a member of the CD28 superfamily, is another important immunosuppressive transmembrane protein expressed on the surface of T cells. PD-1 has two ligands,PD-L1 (also known as CD274 or B7-H1) andPD-L2 (also known as CD273 or B7-DC). PD-L1 is more broadly expressed than PD-L2, and mainly exists in hematopoietic and non-hematopoietic cells, such as epithelial cells, vascular epithelial cells and stromal cells. Moreover, the expression of PD-1 is also induced by proinflammtory cytokine, including Interferon,TNFα andVEGF.
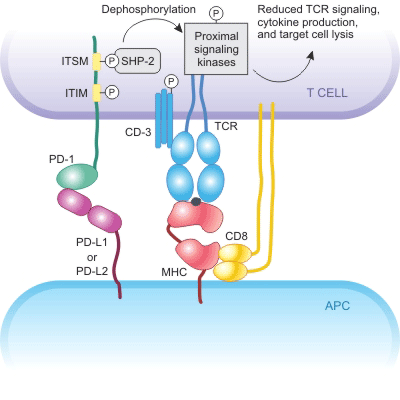
In the microenvironment of the tumor, tumor cells are able to express PD-L1 or PD-L2. Binding of these two ligands to PD-1 results in tyrosine phosphorylation of the intracellular domain of PD-1 and recruitment of tyrosine phosphatase SHP-2, thereby reducing phosphorylation of the TCR signaling pathway, decreasing activation signals downstream of the TCR pathway as well as activation of T cells and production of cytokines. Therefore, inhibition of the PD-1 pathway accelerates and enhances autoimmunity (Figure 2).
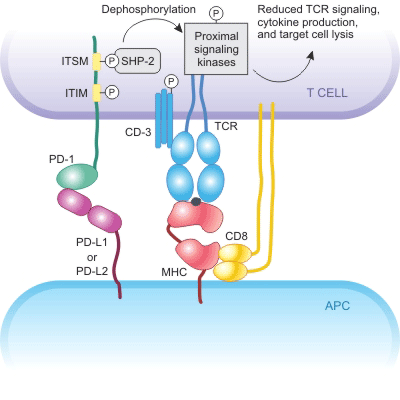
Figure 2. The mechanism of PD-1 inhibits.
CUSABIO team. What Are Immune Checkpoint Inhibitors?. https://www.cusabio.com/c-20761.html




Comments
Leave a Comment