[1] Sallman, David A., et al. "CYAD-01, an autologous NKG2D-based CAR T-cell therapy, in relapsed or refractory a cute myeloid leukaemia and myelodysplastic syndromes or multiple myeloma (THINK): haematological cohorts of the dose escalation segment of a phase 1 trial." The Lancet Haematology 10.3 (2023): e191-e202.
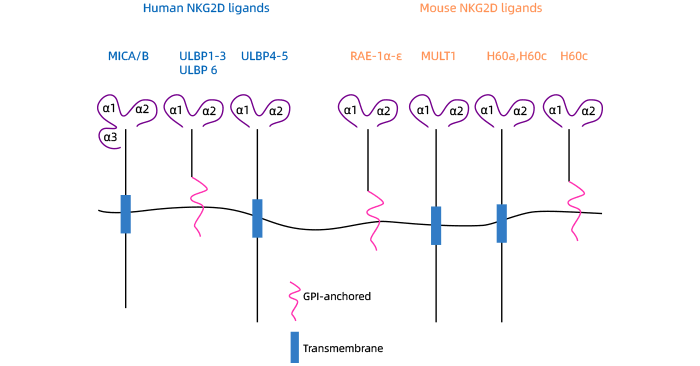
[2] Lanier, Lewis L. "NKG2D receptor and its ligands in host defense." cancer immunology research 3.6 (2015): 575-582.
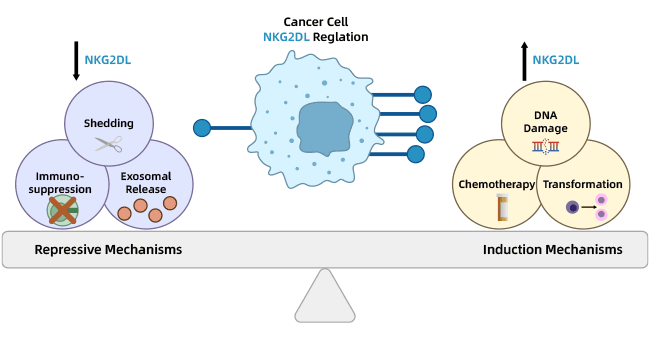
[3] Jones, Amber B., et al. "Regulation of NKG2D stress ligands and its relevance in cancer progression." Cancers 14.9 (2022): 2339.
[4] Baumeister, Susanne H., et al. "Phase I Trial of Autologous CAR T Cells Targeting NKG2D Ligands in Patients with AML/MDS and Multiple MyelomaPhase I Trial of NKG2D-CAR T cells in AML/Myeloma." Cancer immunology research 7.1 (2019): 100-112.
[5] Wu, J., & Wang, X. (2011). NKG2D-Based Cancer Immunotherapy. inTech. doi: 10.5772/23523
[6] Cho, Hanbyoul, et al. "MICA/B and ULBP1 NKG2D ligands are independent predictors of good prognosis in cervical cancer." BMC cancer 14 (2014): 1-11.
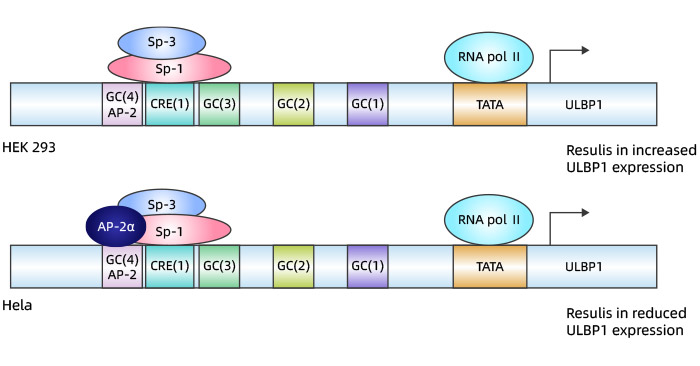
[7] López-Soto, Alejandro, et al. "Transcriptional regulation of ULBP1, a human ligand of the NKG2D receptor." Journal of Biological Chemistry 281.41 ( 2006): 30419-30430.
[8] Ma, H. F., et al. "The construction of reporter plasmid of ULBP1 and preliminary studying on the influence of NS3/4A on transcription of ULBP1." Xi bao yu fen zi Mian yi xue za zhi= Chinese Journal of Cellular and Molecular Immunology 25.6 (2009): 483-485.
[9] Dong Liang, et al. "IL-15 inhibits migration and invasion of esophageal cancer cells by activating NK cell ULBP1/NKG2D signaling in co-culture system." Chinese Journal of Immunology 39.03: 466.
[10] Hu, Baoguang, et al. "Epithelial-mesenchymal transition may be involved in the immune evasion of circulating gastric tumor cells via downregulation of ULBP1." Cancer Medicine 9.8 (2020): 2686-2697.
[11] Qi, Feng, et al. "Tumor mutation burden-associated LINC00638/miR-4732-3p/ULBP1 axis promotes immune escape via PD-L1 in hepatocellular carcinoma." Frontiers in Oncology 11 (2021): 729340.
[12] Textor, Sonja, et al. "Human NK Cells Are Alerted to Induction of p53 in Cancer Cells by Upregulation of the NKG2D Ligands ULBP1 and ULBP2ULBP1 and ULBP2 Are Direct p53 Target Genes." Cancer research 71.18 (2011): 5998-6009.
[13] Nanbakhsh, Arash, et al. "c-Myc regulates expression of NKG2D ligands ULBP1/2/3 in AML and modulates their susceptibility to NK-mediated lysis." Blood , The Journal of the American Society of Hematology 123.23 (2014): 3585-3595.
[14] Jung, Tae-Young, et al. "Immunological characterization of glioblastoma cells for immunotherapy." Anticancer research 33.6 (2013): 2525-2533.
[15] Choi, Haeyoun, et al. "Human allogenic γδ T cells kill patient-derived glioblastoma cells expressing high levels of DNAM-1 ligands. "OncoImmunology 11.1 (2022): 2138152.
[16] Sutherland, Claire L., et al. "ULBPs, human ligands of the NKG2D receptor, stimulate tumor immunity with enhancement by IL-15." Blood 108.4 (2006): 1313 -1319.
[17] Morgado, Sara, et al. "NK cell recognition and killing of melanoma cells is controlled by multiple activating receptor-ligand interactions." Journal of innate immunity 3.4 (2011): 365-373.
[18] Cho, Hanbyoul, et al. "MICA/B and ULBP1 NKG2D ligands are independent predictors of good prognosis in cervical cancer." BMC cancer 14 (2014): 1-11.
[19] Carlsten, Mattias, et al. "DNAX accessory molecule-1 mediated recognition of freshly isolated ovarian carcinoma by resting natural killer cells." Cancer research 67.3 (2007): 1317-1325.
[20] Saito, Hiroki, et al. "A combined lymphokine-activated killer (LAK) cell immunotherapy and adenovirus-p53 gene therapy for head and neck squamous cell carcinoma." Anticancer research 34.7 (2014): 3365-3370.
[21] Kim, So-Jung, et al. "COX-2- and endoplasmic reticulum stress-independent induction of ULBP-1 and enhancement of sensitivity to NK cell-mediated cytotoxicity by celecoxib in colon cancer cells." Experimental Cell Research 330.2 (2015): 451-459.
[22] Chen, Jiong, et al. "Expression and prognostic significance of unique ULBPs in pancreatic cancer." OncoTargets and therapy (2016): 5271-5279.
[23] Textor, Sonja, et al. "Human NK Cells Are Alerted to Induction of p53 in Cancer Cells by Upregulation of the NKG2D Ligands ULBP1 and ULBP2ULBP1 and ULBP2 Are Direct p53 Target Genes." Cancer research 71.18 (2011): 5998-6009.
[24] Lanca, Telma, et al. "The MHC class Ib protein ULBP1 is a nonredundant determinant of leukemia/lymphoma susceptibility to γδ T-cell cytotoxicity." Blood, The Journal of the American Society of Hematology 115.12 (2010): 2407-2411.




Comments
Leave a Comment