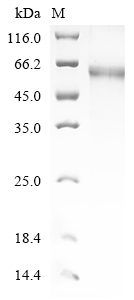
The recombinant human TSHR protein is produced by cloning the TSHR gene with the C-terminal 10xHis tag gene into an expression vector. After transformation into baculovirus, the vectors are induced to express as TSHR protein using IPTG. The recombinant TSHR protein is extracted and purified by Ni-NTA affinity chromatography. The His tag on the protein allows for selective binding to nickel ions, ensuring efficient purification. The TSHR protein is then analyzed via SDS-PAGE, showing a purity level of over 90%.
The human TSHR is a critical component of the hypothalamic-pituitary-thyroid (HPT) axis, functioning primarily as a GPCR that mediates the effects of thyroid-stimulating hormone (TSH) on thyroid follicular cells [1][2]. TSHR is predominantly expressed in the thyroid gland, where it plays a pivotal role in regulating thyroid hormone synthesis and secretion.
The activation of TSHR by TSH initiates a cascade of intracellular signaling pathways, primarily involving the Gs and Gq proteins, which lead to the production of cAMP and the mobilization of intracellular calcium, respectively. This signaling is crucial for the synthesis of thyroid hormones, T3 and T4, which are essential for metabolic regulation [3][4]. Dysregulation of TSHR signaling is implicated in several thyroid disorders, particularly autoimmune conditions such as Graves' disease, where autoantibodies against TSHR stimulate excessive thyroid hormone production, resulting in hyperthyroidism [5-7]. Mutations in the TSHR gene can lead to congenital hypothyroidism and other thyroid dysgenesis syndromes, underscoring the receptor's critical role in thyroid development and function [12].
References:
[1] J. Morillo-Bernal, J. Fernández-Santos, J. Utrilla, M. Miguel, R. García-Marín, & I. Martín-Lacave, Functional expression of the thyrotropin receptor in c cells: new insights into their involvement in the hypothalamic‐pituitary‐thyroid axis, Journal of Anatomy, vol. 215, no. 2, p. 150-158, 2009. https://doi.org/10.1111/j.1469-7580.2009.01095.x
[2] A. Haas, G. Kleinau, I. Hoyer, S. Neumann, J. Furkert, C. Rutz, et al. Mutations that silence constitutive signaling activity in the allosteric ligand-binding site of the thyrotropin receptor, Cellular and Molecular Life Sciences, vol. 68, no. 1, p. 159-167, 2010. https://doi.org/10.1007/s00018-010-0451-2
[3] X. Cheng, Receptor modulators associated with the hypothalamus -pituitary-thyroid axis, Frontiers in Pharmacology, vol. 14, 2023. https://doi.org/10.3389/fphar.2023.1291856
[4] B. Faust, I. Singh, K. Zhang, N. Hoppe, A. Pinto-Duarte, Y. Muftuoglu, et al. Autoantibody and hormone activation of the thyrotropin g protein-coupled receptor, 2022. https://doi.org/10.1101/2022.01.06.475289
[5] A. Budavari, M. Whitaker, & R. Helmers, Thymic hyperplasia presenting as anterior mediastinal mass in 2 patients with graves disease, Mayo Clinic Proceedings, vol. 77, no. 5, p. 495-499, 2002. https://doi.org/10.4065/77.5.495
[6] M. Ahmed, Outcomes of long-term follow-up of patients receiving antithyroid medication for hyperthyroidism due to graves' disease, The Scientific Journal of Medical Scholar, p. 54-63, 2023. https://doi.org/10.55675/sjms.v2i2.47
[7] M. Jin, A. Jang, C. Kim, T. Kim, W. Kim, Y. Shong, et al. Long-term follow-up result of antithyroid drug treatment of graves’ hyperthyroidism in a large cohort, European Thyroid Journal, vol. 12, no. 2, 2023. https://doi.org/10.1530/etj-22-0226
[8] M. Castanet, S. Sura-Trueba, A. Chauty, A. Carré, N. Roux, S. Heath, et al. Linkage and mutational analysis of familial thyroid dysgenesis demonstrate genetic heterogeneity implicating novel genes, European Journal of Human Genetics, vol. 13, no. 2, p. 232-239, 2004. https://doi.org/10.1038/sj.ejhg.5201321