Cancer is the second leading cause of death in the world, with an estimated 9.6 million people worldwide dying of cancer in 2018. Globally, about one in six deaths are due to cancer. The
number of people who die from cancer every year is also increasing year by year. It is not an exaggeration to compare cancer to the murderer who does not see blood.
Cancer is a disease caused by the loss of normal regulation and excessive proliferation of cells in the body. With the improvement of living standards and environmental pollution, various types of
cancer are emerging. Unfortunately, there are currently no effective drugs or treatments for cancer.
In normal condition, our immune system is able to detect and destroy cancer cells. But some tumor cells cleverly escaped the immune system so that they could survive without being identified.
This process is called immune escape. In addition, some cancer cells can also weaken the immune system so that it is not enough to identify and kill cancer cells.
Unlike traditional surgeries, chemotherapy, radiotherapy, and targeted therapies, immunotherapy targets, not tumor cells and tissues but the body's own immune system. In this article, we will
introduce immunotherapy from four aspects, its emergence, definition, classification, current application.
1. What is immunotherapy?
Immunotherapy, also known as biological therapy, is a newly emerging cancer treatment that strengthens the immune system or helps it recognize cancers
and destroy them.
2. The emergence of immunotherapy
It is well known that standard treatments for cancer include surgery, chemotherapy, and radiation therapy. With the development of science and technology,
the therapeutic effects of these therapies continue to increase, and the side effects are decreasing, but it is far from perfect. Patients suffering from cancer pain, but they also often bear the pain of
treatments. A considerable number of advanced patients have reached the point of no drugs or cure.
However, immunotherapy has achieved some good therapeutic effects on certain cancers, making hopeless patients see hope. At this time, immunotherapy
slowly entered the public eye.
In recent years, immunotherapy has been enjoyed as the fourth largest therapy after surgery, radiotherapy, and chemotherapy in the field of cancer
treatment.
3. Classification of immunotherapy
3.1 Immune checkpoint inhibitors
Immune checkpoint therapy is a way that treats cancer homed in on immune checkpoints. Immune checkpoints are molecules that can inhibit receptors and signaling pathways, and thus
normally suppressing the function of T cells, and may be immune to escape by tumor utilization in tumor tissues.
Checkpoint proteins are a series of proteins
encoded by checkpoint genes. Checkpoint inhibitors are monoclonal antibodies that enable
immune system cells to attack and kill cancer cells by blocking checkpoint proteins. Currently, there are three kinds of foreign drugs on the market, including PD-1 inhibitors, PD-L1 inhibitors, and CTLA-4
inhibitors.
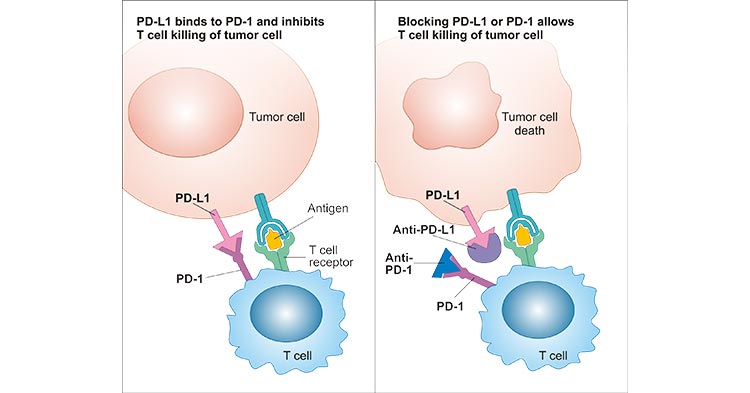
* PD-1PD-L1 inhibitor
PD-1PD-L1 proteins are normally used to prevent immune cells from accidentally injuring normal cells. PD-L1 (programmed death ligand 1) is expressed on the surface of normal cells and PD-1 (programmed death 1) is expressed on the
surface of immune cells. These two are like a pair of mandarin ducks. When the PD-1 protein binds to the PD-L1 protein attached to normal cells or cancer cells, they tell the immune cells not to attack these
cells.
But this mechanism has been learned by some clever cancer cells, and it has become a key routine for cancer cells to suppress immune cells. Cancer cells
bind to PD-1 on the surface of immune cells by expressing a large amount of PD-L1 protein, thereby deceiving immune cells and transmitting a false signal the other is a good cell, don't kill it.
PD-1 inhibitors and PD-L1 inhibitors work in a similar way, which is to forcibly disassemble the combination of PD-1 and PD-L1. After this binding is
eliminated, immune cells begin to recognize the cancer cells and destroy them.
Figure 1: PD-1PD-L1 pathway
(sourcing: httpsmosmedpreparaty.runews15636)
* CTLA-4 inhibitor
Cytotoxic T-lymphocyte protein 4, also known as CTLA-4, is another protein found in immune cells that act as a switch off. CTLA-4 acts on the initiation phase of the immune response, and its activation inhibits the
initiation of the T cell immune response, resulting in a decrease in activated T cells and prevention of memory T cell production. Ipilimumab is an antibody attached on its surface.
3.2 Therapeutic antibody
Therapeutic antibodies are laboratory-synthesized antibodies that destroy tumor cells, attempting to kill tumor cells through different pathways, including
antibody-dependent cell-mediated cytotoxicity (ADCC), complement-dependent Cytotoxicity (complement-dependent cytotoxicity, CDC) and antibodies directly induce apoptosis.
3.3 Non-specific immunotherapy
Non-specific immunotherapy is previously called immune system modulators, which widely promotes the immune system to better respond to tumor cells.
Non-specific immunotherapy includes interleukin and interferon. IL2 (interleukin 2) is used to
treat kidney cancer and skin cancer, such as melanoma. IFNA2 (interferon alpha 2) is the
most common interferon applied in the cancer treatments.
3.4 Cancer vaccine
As all we know, vaccinating healthy people is to prevent infections such as measles and chickenpox. These vaccines use weakened or killed germs, such as
viruses or bacteria, to initiate an immune response in the body. Preparing the immune system to defend against these bacteria helps prevent infection.
Some cancer vaccines work the same way, but they make the immune system attack cancer cells. These cancer vaccines are called preventive vaccines. For
example, HPV (human papilloma virus) vaccine may prevent cervical cancer, anal cancer, and laryngeal cancer. HBV (hepatitis B virus) vaccine help prevent hepatitis B virus infection may reduce the risk of
liver cancer in some people.
Another type is therapeutic vaccines. Cancer treatment vaccines are different from vaccines for viruses. These vaccines try to get the immune system to
attack cancer cells in the body. Instead of preventing disease, they let the immune system attack an existing disease.
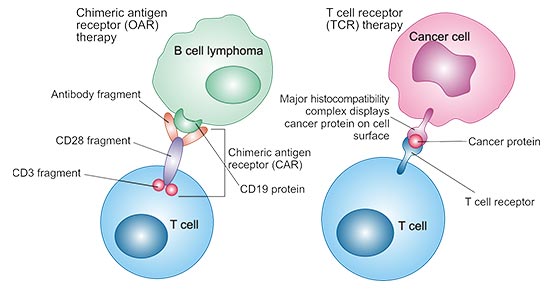
3.5 CAR T-cell therapy
CAR T-cell therapy, short for chimeric antigen receptor T-cell therapy, is also called adoptive T cell transfer (ACT). T cells are one type of immune cells
which can fight infections. In this therapy, the T cells removed from the cancer patients are genetically modified in the lab, and then the altered T cells are reintroduced into the patients via intravenous
injection. When they are ready, they start searching and attacking cancer cells.
Figure 2 : CAR T-cell therapy
(sourcinghttpswww.pharmaceutical-journal.comnews-and-analysisfeaturest-cell-therapies-for-cancer-from-outsider-to-pharmaceutical-
darling20201573.article)
4. Current application of immunotherapy
In February 2019, the US FDA approved PD-1 tumor immunotherapy Keytruda for adjuvant treatment of patients with lymph node involvement in melanoma
after complete surgical resection.
On March 29, 2019, China National Drug Administration officially has approved the PD-1 inhibitor drug pembrolizumab produced by Merck combined with
pemetrexed and platinum-based chemotherapy is applicable to the first-line treatment of the epidermal growth factor receptor (EGFR) mutations negative and anaplastic lymphoma kinase (ALK) negative metastatic squamous non-small cell lung cancer (NSCLC). so far, pembrolizumab is the first
and only PD-1 inhibitor approved by the Chinese Drug Administration to expand the range of adaptive cancers.
Currently, two CTLA-4 inhibitors, Ipilimumab, have been approved by the FDA for the adjuvant treatment of stage III melanoma and the treatment of
advanced melanoma, and clinical studies of Ipilimumab and Tremelimumab in kidney cancer, prostate cancer, and lung cancer have been widely carried out. Early clinical studies have shown that both
monoclonal antibodies are safe and effective, either monotherapy or in combination with IL2, PD-1PD-L1 inhibitors or chemotherapy.
So who can benefit from immunotherapy At present, the international mainstream screening method including the detection of specific molecular markers of
immune checkpoints by IHC immunohistochemistry through pathology is used to screen patients.
Although many experts and doctors are optimistic about the prospect of immunotherapy against cancer, it is still too early to tell whether the medical
treatment in this field will cure cancer forever.
In short-term studies, there are safe and effective effects in many treatments. But it is unknown about long-term risks or late effects. Still, many patients
find the benefits of treatments outweigh the potential risks.
These findings also need to be validated on a larger patient, but there is a reason to believe that cancer immunization and precision medicine will definitely
get closer to us.
CUSABIO team. Immunotherapy to treat cancer. https://www.cusabio.com/c-20888.html



Comments
Leave a Comment