[1] Tu, Zhenbo, et al. "CCR9 in cancer: oncogenic role and therapeutic targeting." Journal of hematology & oncology 9.1 (2016): 1-9.
[2] Huber, Max E., et al. "A chemical biology toolbox targeting the intracellular binding site of CCR9: fluorescent ligands, new drug leads and PROTACs." Angewandte Chemie International Edition 61.12 (2022): e202116782.
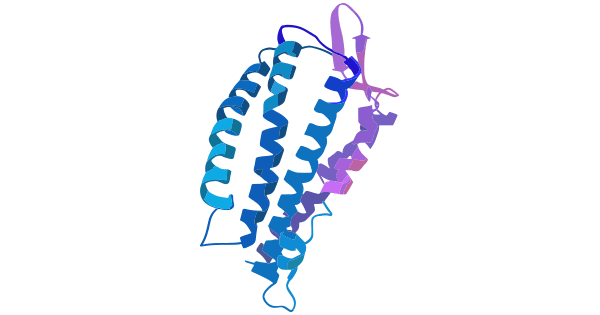
[3] Oswald, Christine, et al. "Intracellular allosteric antagonism of the CCR9 receptor." Nature 540.7633 (2016): 462-465.
[4] Letsch, Anne, et al. "Functional CCR9 expression is associated with small intestinal metastasis." Journal of Investigative Dermatology 122.3 (2004): 685-690.
[5] Uehara, Shoji, et al. "Characterization of CCR9 expression and CCL25/thymus-expressed chemokine responsiveness during T cell development: CD3highCD69+ thymocytes and γδTCR+ thymocytes preferentially respond to CCL25." The Journal of Immunology 168.1 (2002): 134-142.
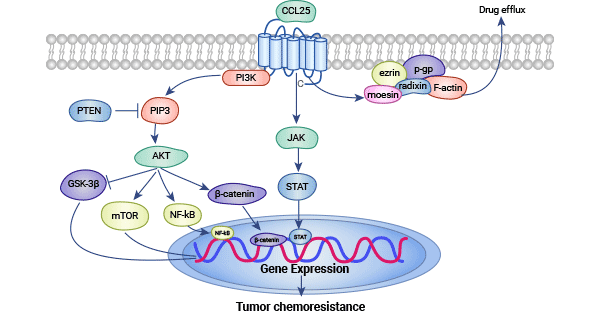
[6] Xu, Baoping, et al. "CCR9 and CCL25: A review of their roles in tumor promotion." Journal of cellular physiology 235.12 (2020): 9121-9132.
[7] Wu, Xue, et al. "The roles of CCR9/CCL25 in inflammation and inflammation-associated diseases." Frontiers in cell and developmental biology 9 (2021): 686548.
[8] Mir, Hina, and Shailesh Singh. "CCL25 signaling in the tumor microenvironment." Tumor Microenvironment: The Role of Chemokines–Part B (2021): 99-111.
[9] Wang, Cong, et al. "The role of chemokine receptor 9/chemokine ligand 25 signaling: From immune cells to cancer cells." Oncology letters 16.2 (2018): 2071-2077.
[10] Li, Baijun, et al. "CCR9–CCL25 interaction suppresses apoptosis of lung cancer cells by activating the PI3K/Akt pathway." Medical Oncology 32 (2015): 1-9.
[11] Sharma, Praveen K., et al. "CCR9 mediates PI3K/AKT‐dependent antiapoptotic signals in prostate cancer cells and inhibition of CCR9‐CCL25 interaction enhances the cytotoxic effects of etoposide." International journal of cancer 127.9 (2010): 2020-2030.
[12] Chai, Songling, et al. "CCL25/CCR9 interaction promotes the malignant behavior of salivary adenoid cystic carcinoma via the PI3K/AKT signaling pathway." PeerJ 10 (2022): e13844.
[13] Johnson-Holiday, Crystal, et al. "CCR9-CCL25 interactions promote cisplatin resistance in breast cancer cell through Akt activation in a PI3K-dependent and FAK-independent fashion." World journal of surgical oncology 9.1 (2011): 1-7.
[14] Soldevila, Gloria, and Eduardo A. García‐Zepeda. "The role of the Jak‐Stat pathway in chemokine‐mediated signaling in T lymphocytes." Signal Transduction 7.5‐6 (2007): 427-438.
[15] Lu, Jianming, et al. "The selective CCR9 antagonist CCX8037 inhibits CCL25-CCR9-STAT3 mediated proliferation of pancreatic cancer cells." Cancer Research 70.8_Supplement (2010): 2531-2531.
[16] Santamaria, Silvia, et al. "Therapeutic potential of an anti-CCR9 mAb evidenced in xenografts of human CCR9+ tumors." Frontiers in Immunology 13 (2022): 825635.
[17] Qiuping, Zhang, et al. "Selectively increased expression and functions of chemokine receptor CCR9 on CD4+ T cells from patients with T-cell lineage acute lymphocytic leukemia." Cancer research 63.19 (2003): 6469-6477.
[18] Mirandola, Leonardo, et al. "Notch1 regulates chemotaxis and proliferation by controlling the CC‐chemokine receptors 5 and 9 in T cell acute lymphoblastic leukaemia." The Journal of pathology 226.5 (2012): 713-722.
[19] Amersi, Farin F., et al. "Activation of CCR9/CCL25 in cutaneous melanoma mediates preferential metastasis to the small intestine." Clinical cancer research 14.3 (2008): 638-645.
[20] Singh, Shailesh, et al. "Expression and functional role of CCR9 in prostate cancer cell migration and invasion." Clinical cancer research 10.24 (2004): 8743-8750.
[21] Sharma, Praveen K., et al. "CCR9 mediates PI3K/AKT‐dependent antiapoptotic signals in prostate cancer cells and inhibition of CCR9‐CCL25 interaction enhances the cytotoxic effects of etoposide." International journal of cancer 127.9 (2010): 2020-2030.
[22] Johnson, Erica L., et al. "CCL25-CCR9 interaction modulates ovarian cancer cell migration, metalloproteinase expression, and invasion." World journal of surgical oncology 8.1 (2010): 1-10.
[23] Singh, Rajesh, et al. "Expression and histopathological correlation of CCR9 and CCL25 in ovarian cancer." International journal of oncology 39.2 (2011): 373-381.
[24] Zhang, Ziqi, et al. "CCL25/CCR9 signal promotes migration and invasion in hepatocellular and breast cancer cell lines." DNA and cell biology 35.7 (2016): 348-357.
[25] Johnson-Holiday, Crystal, et al. "CCL25 mediates migration, invasion and matrix metalloproteinase expression by breast cancer cells in a CCR9-dependent fashion." International journal of oncology 38.5 (2011): 1279-1285.
[26] Johnson-Holiday, Crystal, et al. "CCR9-CCL25 interactions promote cisplatin resistance in breast cancer cell through Akt activation in a PI3K-dependent and FAK-independent fashion." World journal of surgical oncology 9.1 (2011): 1-7.
[27] Shen, Xiaoming, et al. "CC chemokine receptor 9 enhances proliferation in pancreatic intraepithelial neoplasia and pancreatic cancer cells." Journal of Gastrointestinal Surgery 13 (2009): 1955-1962.
[28] Heinrich, Eileen L., et al. "Paracrine activation of chemokine receptor CCR9 enhances the invasiveness of pancreatic cancer cells." Cancer Microenvironment 6 (2013): 241-245.
[29] Lu, Lin, et al. "CCR9 promotes migration and invasion of lung adenocarcinoma cancer stem cells." International journal of medical sciences 17.7 (2020): 912.
[30] Zhong, Yonglong, et al. "Expression of CC chemokine receptor 9 predicts poor prognosis in patients with lung adenocarcinoma." Diagnostic pathology 10.1 (2015): 1-7.
[31] Fan, Jian, et al. "Chemokine receptor 9 high-expression involved in the migration and invasion of the non-small-cell lung cancer cells."Asian Biomedicine 5.1 (2011): 69-76.
[32] Gupta, Pranav, et al. "CCR9/CCL25 expression in non-small cell lung cancer correlates with aggressive disease and mediates key steps of metastasis." Oncotarget 5.20 (2014): 10170.
[33] Li, Baijun, et al. "CCR9–CCL25 interaction suppresses apoptosis of lung cancer cells by activating the PI3K/Akt pathway." Medical Oncology 32 (2015): 1-9.
[34] Niu, Yuxu, et al. "CCL25 promotes the migration and invasion of non‑small cell lung cancer cells by regulating VEGF and MMPs in a CCR9‑dependent manner." Experimental and Therapeutic Medicine 19.6 (2020): 3571-3580.
[35] Zhang, Zhenhai, et al. "CCR9 as a prognostic marker and therapeutic target in hepatocellular carcinoma." Oncology Reports 31.4 (2014): 1629-1636.
[36] Amersi, Farin F., et al. "Activation of CCR9/CCL25 in cutaneous melanoma mediates preferential metastasis to the small intestine." Clinical cancer research 14.3 (2008): 638-645.
[37] Kühnelt-Leddihn, Laura, et al. "Overexpression of the chemokine receptors CXCR4, CCR7, CCR9, and CCR10 in human primary cutaneous melanoma: a potential prognostic value for CCR7 and CCR10?." Archives of dermatological research 304 (2012): 185-193.
[38] Richmond, Ann. "CCR9 homes metastatic melanoma cells to the small bowel." Clinical Cancer Research 14.3 (2008): 621-623.
[39] Hwang, Sam T. "Chemokine receptors in melanoma: CCR9 has a potential role in metastasis to the small bowel." J invest Dermatol 122.3 (2004): 14-15.
[40] Van Den Oord, Joost. "The CCR9–CCL25 axis mediates melanoma metastasis to the small intestine." Nature clinical practice Oncology 5.8 (2008): 440-441.




Comments
Leave a Comment