Chemokines are a series of cytokines with small molecular weight whose main role is the recruitment of leukocyte subsets under homeostatic and pathological conditions. Their name is derived from their ability to induce directed chemotaxis in nearby responsive cells; they are chemotactic cytokines.
Trough interacting with chemokine receptors that are expressed on the cell surface as 7-transmembrane proteins coupled with G-protein for signaling transduction, chemokines can induce firm adhesion of targeted cells to the endothelium and direct the movement of targeted cells to their destination according to the concentration gradient of a given chemokine. In this article, we introduce the family of chemokines and receptors, its key role in the inflammation, and so on.
1. The Function of Chemokines
The major role of chemokines is to act as a chemoattractant to guide the migration of cells. Cells that are attracted by chemokines follow a signal of increasing chemokine concentration towards the source of the chemokine.
The function of chemokines are divided into two sections. One of them is homeostatic, which are constitutively produced in certain tissues and are responsible for basal leukocyte migration. These include: CCL14, CCL19, CCL20, CCL21, CCL25, CCL27, CXCL12 and CXCL13. This classification is not strict; for example, CCL20 can act also as pro-inflammatory chemokine. Another is inflammatory, which are formed under pathological conditions (on pro-inflammatory stimuli, such as IL-1, TNF-alpha, LPS, or viruses) and actively participate in the inflammatory response attracting immune cells to the site of inflammation. Examples are: CXCL-8, CCL2, CCL3, CCL4, CCL5, CCL11, CXCL10.
2. The types of Chemokines and Chemokine Receptors
Chemokines are a group of cytokines with small molecular weight whose main action is the recruitment of leukocyte subsets under homeostatic and pathological conditions.
Through interacting with chemokine receptors that are expressed on the cell surface as 7-transmembrane proteins coupled with G-protein for signaling transduction, chemokine can induce firm adhesion of targeted cells to the endothelium and direct the movement of targeted cells to their destination according to the concentration gradient of a given chemokine. According to behavior and structural characteristics, the chemokine family consists of 50 endogenous chemokine ligands in humans and mice (Table 1) [1][2][3][4][5][6].
Table 1a. CC chemokines
|
Name
|
Protein Name
|
Other name(s)
|
Receptor
|
Uniprot ID
|
|
CCL1
|
C-C motif chemokine 1
|
I-309, TCA-3
|
CCR8
|
P22362
|
|
CCL2
|
C-C motif chemokine 2
|
MCP-1
|
CCR2
|
P13500
|
|
CCL3
|
C-C motif chemokine 3
|
MIP-1a
|
CCR1
|
P10147
|
|
CCL4
|
C-C motif chemokine 4
|
MIP-1β
|
CCR1, CCR5
|
P13236
|
|
CCL5
|
C-C motif chemokine 5
|
RANTES
|
CCR5
|
P13501
|
|
CCL6
|
C-C motif chemokine 6
|
C10, MRP-2
|
CCR1
|
P27784
|
|
CCL7
|
C-C motif chemokine 7
|
MARC, MCP-3
|
CCR2
|
P80098
|
|
CCL8
|
C-C motif chemokine 8
|
MCP-2
|
CCR1, CCR2B, CCR5
|
P80075
|
|
CCL9/CCL10
|
C-C motif chemokine 9
|
MRP-2, CCF18, MIP-1?
|
CCR1
|
P51670
|
|
CCL11
|
Eotaxin
|
C-C motif chemokine 11, Eosinophil chemotactic protein, Small-inducible cytokine A11
|
CCR2, CCR3, CCR5
|
P51671
|
|
CCL12
|
C-C motif chemokine 12
|
MCP-5
|
unknown
|
Q62401
|
|
CCL13
|
C-C motif chemokine 13
|
MCP-4, NCC-1, Ckβ10
|
CCR2, CCR3, CCR5
|
Q99616
|
|
CCL14
|
C-C motif chemokine 14
|
HCC-1, MCIF, Ckβ1, NCC-2, CCL
|
CCR1
|
Q16627
|
|
CCL15
|
C-C motif chemokine 15
|
Leukotactin-1, MIP-5, HCC-2, NCC-3
|
CCR1, CCR3
|
Q16663
|
|
CCL16
|
C-C motif chemokine 16
|
LEC, NCC-4, LMC, Ckβ12
|
CCR1, CCR2, CCR5, CCR8
|
O15467
|
|
CCL17
|
C-C motif chemokine 17
|
TARC, dendrokine, ABCD-2
|
CCR4
|
Q92583
|
|
CCL18
|
C-C motif chemokine 18
|
PARC, DC-CK1, AMAC-1, Ckβ7, MIP-4
|
unknown
|
P55774
|
|
CCL19
|
C-C motif chemokine 19
|
ELC, Exodus-3, Ckβ11
|
CCR7
|
Q99731
|
|
CCL20
|
C-C motif chemokine 20
|
LARC, Exodus-1, Ckβ4
|
CCR6
|
P78556
|
|
CCL21
|
C-C motif chemokine 21
|
SLC, 6Ckine, Exodus-2, Ckβ9, TCA-4
|
CCR7
|
O00585
|
|
CCL22
|
C-C motif chemokine 22
|
MDC, DC/β-CK
|
CCR4
|
O00626
|
|
CCL23
|
C-C motif chemokine 23
|
MPIF-1, Ckβ8, MIP-3, MPIF-1
|
CCR1
|
P55773
|
|
CCL24
|
C-C motif chemokine 24
|
Eotaxin-2, MPIF-2, Ckβ6
|
CCR3
|
O00175
|
|
CCL25
|
C-C motif chemokine 25
|
TECK, Ckβ15
|
CCR9
|
O15444
|
|
CCL26
|
C-C motif chemokine 26
|
Eotaxin-3, MIP-4a, IMAC, TSC-1
|
CCR3
|
Q9Y258
|
|
CCL27
|
C-C motif chemokine 27
|
CTACK, ILC, Eskine, PESKY, skinkine
|
CCR10
|
Q9Y4X3
|
|
CCL28
|
C-C motif chemokine 28
|
MEC
|
CCR3, CCR10
|
Q9NRJ3
|
Table 1b. CXC chemokines
|
Name
|
Protein Name
|
Other name(s)
|
Receptor
|
Uniprot ID
|
|
CXCL1
|
Growth-regulated alpha protein
|
C-X-C motif chemokine 1, Gro-a, GRO1, NAP-3, KC
|
CXCR2
|
P09341
|
|
CXCL2
|
C-X-C motif chemokine 2
|
Gro-β, GRO2, MIP-2a
|
CXCR2
|
P19875
|
|
CXCL3
|
C-X-C motif chemokine 3
|
Gro-?, GRO3, MIP-2β
|
CXCR2
|
P19876
|
|
CXCL4
|
Platelet factor 4
|
PF-4, C-X-C motif chemokine 4, roplact, Oncostatin-A
|
CXCR3B
|
P02776
|
|
CXCL5
|
C-X-C motif chemokine 5
|
ENA-78
|
CXCR2
|
P42830
|
|
CXCL6
|
C-X-C motif chemokine 6
|
GCP-2
|
CXCR1, CXCR2
|
P80162
|
|
CXCL7
|
Platelet basic protein
|
NAP-2, CTAPIII, β-Ta, PEP
|
unknown
|
P02775
|
|
CXCL8
|
Interleukin-8
|
IL-8, NAP-1, MDNCF, GCP-1
|
CXCR1, CXCR2
|
P10145
|
|
CXCL9
|
C-X-C motif chemokine 9
|
MIG, CRG-10
|
CXCR3
|
Q07325
|
|
CXCL10
|
C-X-C motif chemokine 10
|
IP-10, CRG-2
|
CXCR3
|
P02778
|
|
CXCL11
|
C-X-C motif chemokine 11
|
I-TAC, β-R1, IP-9
|
CXCR3, CXCR7
|
O14625
|
|
CXCL12
|
Stromal cell-derived factor 1
|
SDF-1, PBSF
|
CXCR4, CXCR7
|
P48061
|
|
CXCL13
|
C-X-C motif chemokine 13
|
BCA-1, BLC
|
CXCR5
|
O43927
|
|
CXCL14
|
C-X-C motif chemokine 14
|
BRAK, bolekine
|
unknown
|
O95715
|
|
CXCL15
|
C-X-C motif chemokine 15
|
Lungkine, WECHE
|
unknown
|
Q9WVL7
|
|
CXCL16
|
C-X-C motif chemokine 16
|
SRPSOX
|
CXCR6
|
Q9H2A7
|
|
CXCL17
|
C-X-C motif chemokine 17
|
DMC, VCC-1
|
unknown
|
Q6UXB2
|
Table 1c. C chemokines
|
Name
|
Protein Name
|
Other name(s)
|
Receptor
|
Uniprot ID
|
|
XCL1
|
Lymphotactin
|
Lymphotactin a, SCM-1a, ATAC
|
XCR1
|
P47992
|
|
XCL2
|
Cytokine SCM-1 beta
|
Lymphotactin β, SCM-1β
|
XCR1
|
Q9UBD3
|
Table 1d CX3C chemokines
|
Name
|
Protein Name
|
Other name(s)
|
Receptor
|
Uniprot ID
|
|
CX3CL1
|
Fractalkine
|
Fractalkine, Neurotactin, ABCD-3
|
CX3CR1
|
P78423
|
Chemokines are a group of cytokines with small molecular weight whose main action is the recruitment of leukocyte subsets under homeostatic and pathological conditions.
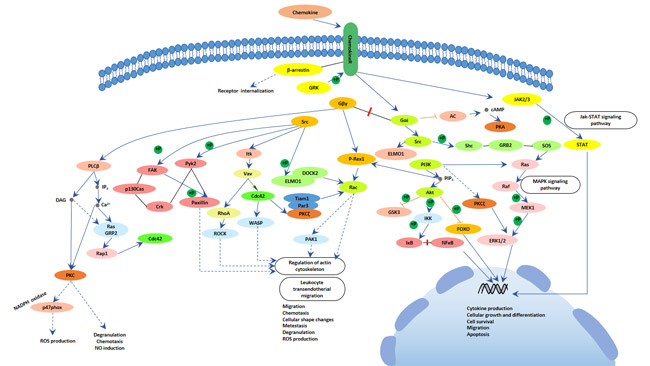
Through interacting with chemokine receptors that are expressed on the cell surface as 7-transmembrane proteins coupled with G-protein to transmit cell signals following ligand binding. Activation of G proteins, by chemokine receptors, causes the subsequent activation of an enzyme known as phospholipase C (PLC). PLC cleaves a molecule called phosphatidylinositol (4,5)-bisphosphate (PIP2) into two second messenger molecules known as Inositol triphosphate (IP3) and diacylglycerol (DAG) that trigger intracellular signaling events; DAG activates another enzyme called protein kinase C (PKC), and IP3 triggers the release of calcium from intracellular stores. These events promote many signaling cascades (such as the MAP kinase pathway) that generate responses like chemotaxis, degranulation, release of superoxide anions and changes in the avidity of cell adhesion molecules called integrins within the cell harbouring the chemokine receptor[7].
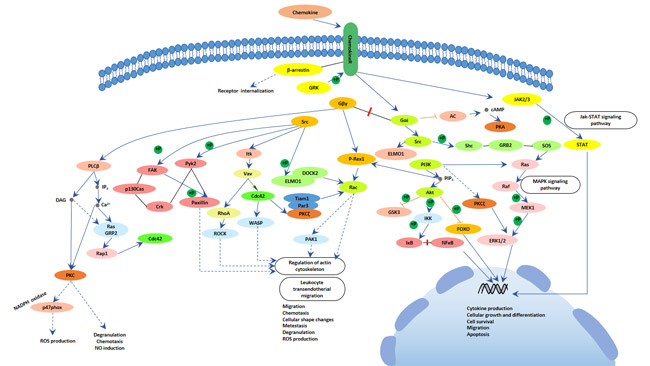
Fig.1. The picture of chemokine signaling pathway
4. Chemokine and inflammation
Chemokines are chemotactic cytokines that direct the movement of circulating leukocytes to sites of inflammation or injury. Originally studied because of their role in inflammation, chemokines and their receptors are now known to play a crucial part in directing the movement of mononuclear cells throughout the body, engendering the adaptive immune response and contributing to the pathogenesis of a variety of diseases. Chemokine receptors are some of the most tractable drug targets in the huge battery of molecules that regulate inflammation and immunity[8][9]. Here, we survey the properties of chemokines and their receptors and highlight the roles of these chemoattractants in selected clinical disorders.
The chemokine system in innate immune cell homeostasis
Maintenance of hematopoietic stem cells and developing innate immune cells takes place largely in the bone marrow (BM) and is dependent on CXCL12/CXCR4 interactions[10]. As immune cell development progresses past the hematopoietic stem cell, CXCL12/CXCR4 interactions remain essential for BM retention and normal development of multiple immune lineages, including B cells, monocytes, macrophages, neutrophils, natural killer (NK) cells, and plasmacytoid dendritic cells[11]. CXCR4-mediated signaling plays a major role in promoting BM retention of many immune cells. However, exit from the BM may not be entirely passive. In studies examining monocyte development and release from the BM, blockade of CXCR4 induces only a small increase in the number of peripheral blood monocytes[12].
The chemokine system in acute inflammation
Acute Inflammation is a general pattern of immune response to cell injury characterized by rapid accumulation of immune cells at the site of injury. The acute inflammatory response is initiated by both immune and parenchymal cells at the site of injury and is coordinated by a wide variety of soluble mediators.
This coordination starts with the homeostatic prepositioning of innate immune cells throughout the periphery, where they act as local sensors of infection and inflammation through the activation of pattern recognition receptors (PRRs), the inflammasome, and/or RNA and DNA sensors. Neutrophils, monocytes, and basophils, almost all innate immune cells are present to some extent in the periphery under homeostatic conditions. There they lie in wait as sensors of pathogen invasion, via PRRs, or tissue damage, via the interleukin (IL)-33 pathway as one example. MCs and macrophages are classically described as essential immune sensors, based on their expression of a wide variety of PRRs and their broad localization throughout all vascularized tissues. MCs are uniquely capable of responding immediately to infectious or inflammatory stimuli. Lipopolysaccharide (LPS) stimulation of murine peritoneal MCs leads to immediate release of CXCL1 and CXCL2-containing granules, but not histamine-containing granules, as well as transcriptional activation of CXCL1 and CXCL2[13].
Inflammatory Diseases
Chemokines have been implicated in a wide range of diseases with prominent inflammatory components. For example, elevated levels of CC chemokines, particularly CCL2, CCL3, and CCL5, in the joints of patients with rheumatoid arthritis coincide with the recruitment of monocytes and T cells into synovial tissues. Inflammation is also a key factor in asthma, in which the chemokine CCL11 (eotaxin) and its receptor, CCR3, contribute to the recruitment of eosinophils to the lung. Psoriasis is another example of chemokine-mediated local cell recruitment and inflammation. Infiltrating effector T cells express CCR4, and its ligands (CCL17 and CCL22) are produced by cutaneous cells. CXCR3 has also been implicated in the recruitment of T cells to inflamed skin[14].
5. The most popular questions about Chemokines
In this part, we enumerate several popular questions about chemokines and hope that may give some help for you.
What is the difference between chemokine and cytokine?
We can differentiate chemokine and cytokines from several aspects. With respect to definition, cytokines are immune-modulating agents which are made up from proteins, while chemokines are a super family of cytokines which mediate chemotaxis. With respect to function, cytokines are involved in both cellular and antibody-mediated immunity in the body, while chemokines are involved in the guiding of cells in the immune system to the site of infection. With respect to types, cytokines include chemokines, ILs, INFs, CSFs, TNFs and TGFs in the body, while chemokines involve CC chemokines, CXC chemokines, C chemokines and CX3C chemokines in the body.
What cells release chemokines?
Some chemokines have roles in development; they promote angiogenesis (the growth of new blood vessels), or guide cells to tissues that provide specific signals critical for cellular maturation. Other chemokines are inflammatory and are released from a wide variety of cells in response to bacterial infection, viruses and agents that cause physical damage such as silica or the urate crystals that occur in gout.
References
[1] Laing KJ, Secombes CJ. Chemokines[J]. Developmental and Comparative Immunology. 2004, 28 (5): 443–60
[2] Villeda SA, Luo J, Mosher KI, et al. The ageing systemic milieu negatively regulates neurogenesis and cognitive function[J]. Nature. 2011, 477 (7362): 90–4
[3] Murdoch C, Finn A. Chemokine receptors and their role in inflammation and infectious diseases[J]. Blood. 2000, 95 (10): 3032–43
[4] Cocchi F, DeVico AL, Garzino-Demo A, et al. Identification of RANTES, MIP-1 alpha, and MIP-1 beta as the major HIV-suppressive factors produced by CD8+ T cells[J]. Science. 1995, 270 (5243): 1811–5
[5] von Recum HA, Pokorski JK. Peptide and protein-based inhibitors of HIV-1 co-receptors[J]. Experimental Biology and Medicine. 2013, 238 (5): 442–9
[6] Garzino-Demo A, Moss RB, Margolick JB, et al. Spontaneous and antigen-induced production of HIV-inhibitory beta-chemokines are associated with AIDS-free status[J]. Proceedings of the National Academy of Sciences of the United States of America. 1999, 96 (21): 11986–91
[7] R. M. Ransohoff. Chemokines and chemokine receptors: standing at the crossroads of immunobiology and neurobiology[J]. Immunity. 2009, 5(31): 711–721
[8] Luster AD. Chemokines — chemotactic cytokines that mediate inflammation[J]. N Engl J Med. 1998, 338:436-45
[9] Israel F. Charo, and Richard M. Ransohoff. The Many Roles of Chemokines and Chemokine Receptors in Inflammation[J]. N Engl J Med. 2006, 354:610-21
[10] Ara T, Tokoyoda K, Sugiyama T, Egawa T, Kawabata K, Nagasawa T. Long-term hematopoietic stem cells require stromal cell-derived factor-1 for colonizing bone marrow during ontogeny[J]. Immunity. 2003, 19: 257–267
[11] Mercier FE, Ragu C, Scadden DT. The bone marrow at the crossroads of blood and immunity[J]. Nat Rev Immunol. 2012, 12: 49–60
[12] Wang Y, Cui L, Gonsiorek W, et al. CCR2 and CXCR4 regulate peripheral blood monocyte pharmacodynamics and link to efficacy in experimental autoimmune encephalomyelitis[J]. J Inflamm (Lond). 2009, 6: 32
[13] Caroline L. Sokol and Andrew D. Luster. The Chemokine System in Innate Immunity[J]. Cold Spring Harb Perspect Biol. 2015, 29:(5)
[14] Flier J, Boorsma DM, van Beek PJ, et al. Differential expression of CXCR3 targeting chemokines CXCL10, CXCL9, and CXCL11 in different types of skin inflammation[J]. J Pathol. 2001, 194:398-405
CUSABIO team. The Overview of Chemokine. https://www.cusabio.com/c-20626.html



Comments
Leave a Comment