[1] Vancamelbeke, M.; Vermeire, S. The intestinal barrier: A fundamental role in health and disease [J]. Expert. Rev. Gastroenterol. Hepatol. 2017, 11, 821–834.
[2] Metta, V.; Leta, V.; et al. Gastrointestinal dysfunction in Parkinson’s disease: Molecular pathology and implications of gut microbiome, probiotics, and fecal microbiota transplantation [J]. J. Neurol. 2021. [Google Scholar] [CrossRef]
[3] DeGruttola, A.K.; Low, D.; et al. Current Understanding of Dysbiosis in Disease in Human and Animal Models [J]. Inflamm. Bowel. Dis. 2016, 22, 1137–1150.
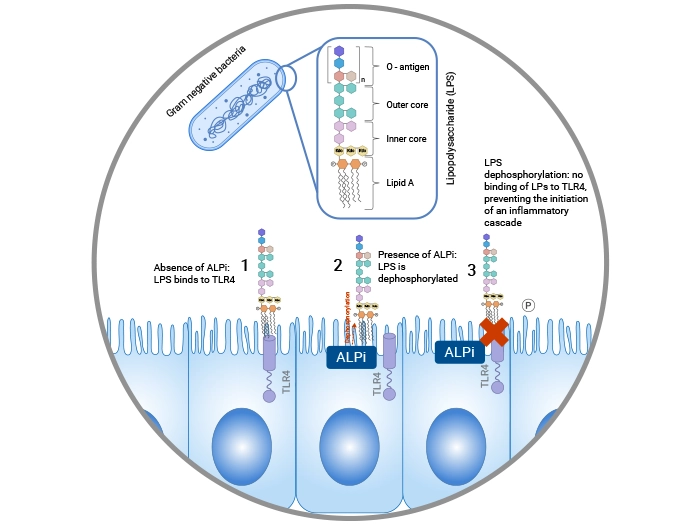
[4] Beumer, C.; Wulferink, M.; et al. Calf intestinal alkaline phosphatase, a novel therapeutic drug for lipopolysaccharide (LPS)-mediated diseases, attenuates LPS toxicity in mice and piglets [J]. J. Pharmacol. Exp. Ther. 2003, 307, 737–744.
[5] Liu, W.; Hu, D.; et al. Intestinal Alkaline Phosphatase Regulates Tight Junction Protein Levels [J]. J. Am. Coll. Surg. 2016, 222, 1009–1017.
[6] Lalles, J.P. Intestinal alkaline phosphatase: Novel functions and protective effects [J]. Nutr. Rev. 2014, 72, 82–94.
[7] Rentea RM, Liedel JL, et al. Intestinal alkaline phosphatase administration in newborns is protective of gut barrier function in necrotizing enterocolitis [J]. J Pediatr Surg. 2012;47(6):1135–1142.
[8] Chen KT, Malo MS, et al. A role for intestinal alkaline phosphatase in the maintenance of local gut immunity [J].Digestive Diseases and Sciences, 56(4), 1020.
[9] Hamarneh SR, Mohamed MM, et al. A novel approach to maintain gut mucosal integrity using an oral enzyme supplement [J]. Ann Surg 2014; 260: 706-14.
[10] Hamarneh, S.R.; Kim, B.M.; et al. Intestinal Alkaline Phosphatase Attenuates Alcohol-Induced Hepatosteatosis in Mice [J]. Dig. Dis. Sci. 2017, 62, 2021–2034.
[11] Dissanayake WMN, Chandanee MR, et al. Change in intestinal alkaline phosphatase activity is a hallmark of antibiotic-induced intestinal dysbiosis [J]. Anim Biosci. 2023 Sep;36(9):1403-1413.
[12] Luo Z, Wang Z, et al. Intestinal alkaline phosphatase improves intestinal permeability and alleviates multiple organ dysfunction caused by heatstroke [J]. Heliyon. 2023 Nov 4;9(11):e21838.
[13] Bentala H, Verweij WR, et al. Removal of phosphate from lipid A as a strategy to detoxify lipopolysaccharide [J]. Shock. 2002;18(6):561–566.
[14] Cario E. Bacterial interactions with cells of the intestinal mucosa [J]. toll-like receptors and NOD2. Gut, 2005, 54( 8): 1182-1193.
[15] Bates JM, Akerlund J, Mittge E, Guillemin K. Intestinal alkaline phosphatase detoxifies lipopolysaccharide and prevents inflammation in zebrafish in response to the gut microbiota [J]. Cell Host Microbe. 2007;2(6):371–382.
[16] Inami A, Kiyono H, Kurashima Y. ATP as a pathophysiologic mediator of bacteria-host crosstalk in the gastrointestinal tract [J]. Int J Mol Sci (2018) 19(8):2371.
[17] Bilski J, Mazur-Bialy A, et al. The role of intestinal alkaline phosphatase in inflammatory disorders of gastrointestinal tract [J]. Mediators Inflamm (2017) 2017:9074601.
[18] Vuerich M, Mukherjee S, Robson SC, Longhi MS. Control of gut inflammation by modulation of purinergic signaling [J]. Front Immunol (2020) 11:1882.
[19] Estaki M, DeCoffe D, Gibson DL. Interplay between intestinal alkaline phosphatase, diet, gut microbes and immunity [J]. World J Gastroenterol (2014) 20(42):15650–6.
[20] Goldberg R. F., Austen W. G., Jr., Zhang X., et al. Intestinal alkaline phosphatase is a gut mucosal defense factor maintained by enteral nutrition [J]. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(9):3551–3556.
[21] Malo M. S., Nasrin Alam S., Mostafa G., et al Intestinal alkaline phosphatase preserves the normal homeostasis of gut microbiota [J]. Gut. 2010;59(11):1476–1484.
[22] Malo M. S., Moaven O., Muhammad N., et al. Intestinal alkaline phosphatase promotes gut bacterial growth by reducing the concentration of luminal nucleotide triphosphates [J]. American Journal of Physiology—Gastrointestinal and Liver Physiology. 2014;306(10):G826–G838.
[23] Lallès J.-P. Luminal ATP: the missing link between intestinal alkaline phosphatase, the gut microbiota, and inflammation [J]? American Journal of Physiology—Gastrointestinal and Liver Physiology. 2014;306(10):G824–G825.
[24] Alam S. N., Yammine H., Ahmed R., et al. Oral supplementation with intestinal alkaline phosphatase: a novel therapy to treat Salmonella colitis [J]. Gastroenterology. 2012;142(5):p. S692.
[25] [8]Mizumori M, Ham M, Guth PH, Engel E, Kaunitz JD, Akiba Y. Intestinal alkaline phosphatase regulates protective surface microclimate pH in rat duodenum [J]. J Physiol. 2009;587(11):2537–2549.
[26] Santos GM, Ismael S, Morais J, Araújo JR, Faria A, Calhau C, Marques C. Intestinal Alkaline Phosphatase: A Review of This Enzyme Role in the Intestinal Barrier Function [J]. Microorganisms. 2022 Mar 30;10(4):746.
[27] Alam SN, Yammine H, et al. Intestinal alkaline phosphatase prevents antibiotic-induced susceptibility to enteric pathogens [J]. Proc Natl Acad Sci U S A. 2014;111(15):5678–5683.
[28] Martins RDS, Hulscher JBF, Timmer A, Kooi EMW, Poelstra K. Necrotizing enterocolitis: a potential protective role for intestinal alkaline phosphatase as lipopolysaccharide detoxifying enzyme [J]. Front Pediatr. 2024 Apr 30;12:1401090.
[29] Martins RDS, Kooi EMW, Poelstra K, Hulscher JBF. The role of intestinal alkaline phosphatase in the development of necrotizing enterocolitis [J]. Early Hum Dev. 2023 Aug;183:105797.
[30] Whitehouse JS, Riggle KM, Purpi DP, Mayer AN, Pritchard KA Jr, Oldham KT, Gourlay DM. The protective role of intestinal alkaline phosphatase in necrotizing enterocolitis [J]. J Surg Res. 2010 Sep;163(1):79-85.
[31] Pickkers, P., Heemskerk, S., et al. (2012). Alkaline phosphatase for treatment of sepsis-induced acute kidney injury: A prospective randomized double-blind placebo-controlled trial [J]. Critical Care, 16(1), R14.
[32] Kaliannan K, Hamarneh SR, et al. Intestinal alkaline phosphatase prevents metabolic syndrome in mice [J]. Proceedings of the National Academy of Sciences of the United States of America, 2013;110(17), 7003.
[33] Goldberg RF, Austen WG Jr, et al. Intestinal alkaline phosphatase is a gut mucosal defense factor maintained by enteral nutrition [J]. Proceedings of the National Academy of Sciences of the United States of America, 105(9), 3551.



Comments
Leave a Comment