What Is Renin-angiotensin System?
The renin-angiotensin system (RAS), also called the renin-angiotensin-aldosterone system (RAAS), is an important body fluid regulatory system. It is found not only in the circulatory system but also in the vascular wall, heart, center, kidney, adrenal, and other tissues.
The Composition of Renin-angiotensin System
As the name implies, there are two key components to this system: renin, angiotensin. There is another hormone aldosterone in the whole process. Renin is a proteolytic enzyme that secreted primarily by the kidneys. It stimulates the formation of angiotensin in blood and tissues. Angiotensin further induces the release of aldosterone from the adrenal cortex.
The Function of Renin-angiotensin System
The Renin-angiotensin system functions to elevate blood volume and arterial tone in a long-term manner. It plays an important role in the normal development of the cardiovascular system, cardiovascular homeostasis, maintenance of electrolyte and fluid balance, and regulation of blood pressure.
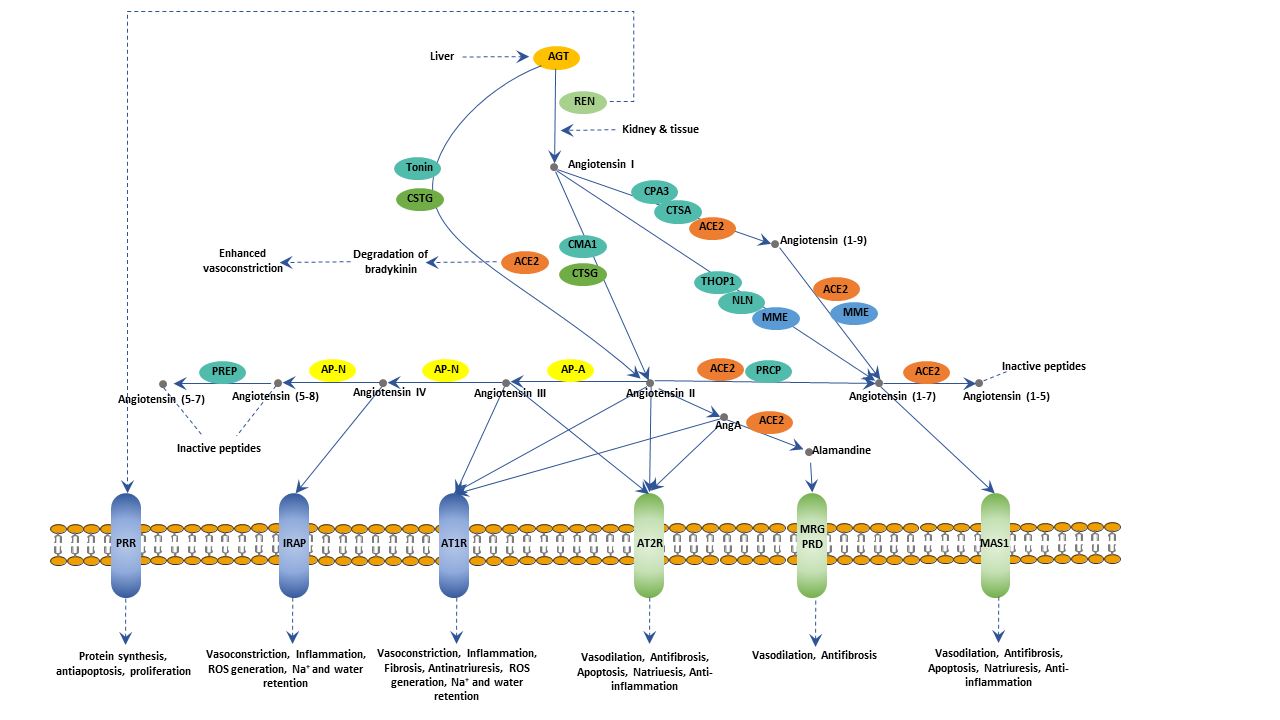
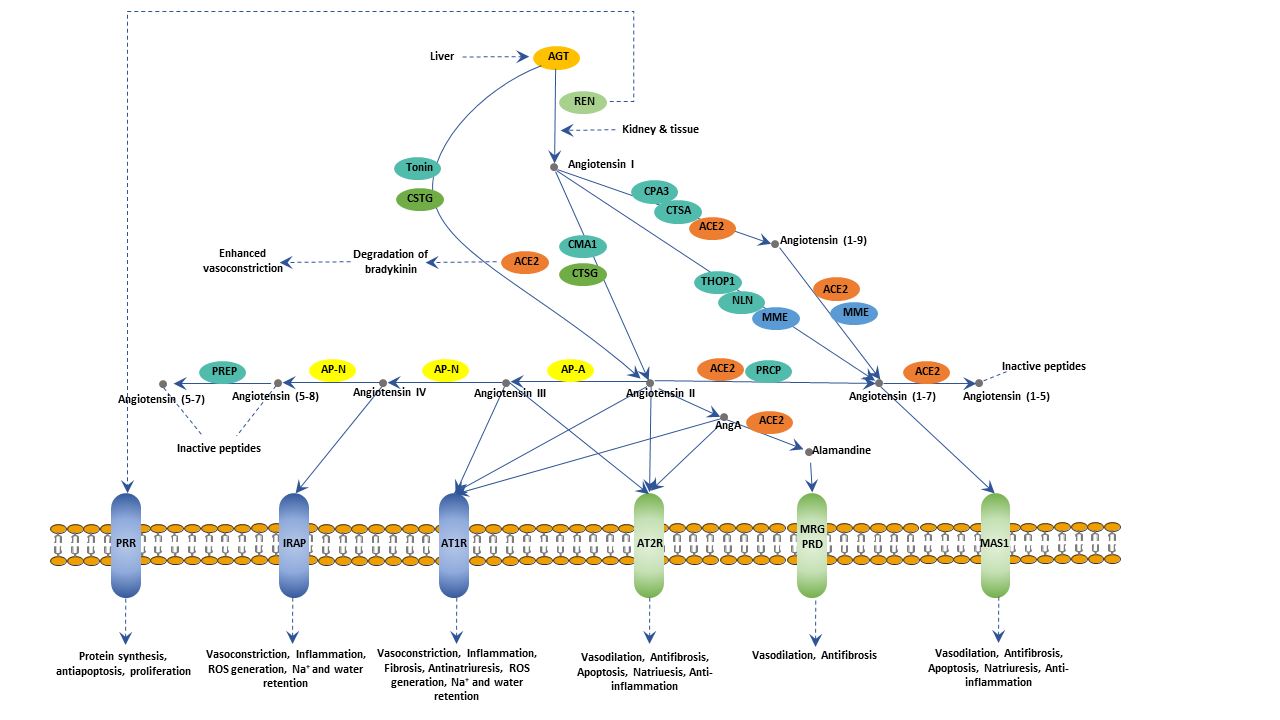
The Renin-angiotensin Pathway
The Renin-angiotensin system is activated when the blood pressure is too low or blood volume loss. When the body senses the blood pressure is too low, the sympathetic nervous system will send nerve impulses to the juxtaglomerular cells in the kidneys. These cells will release renin.
When renin enters the circulation, it acts to convert angiotensinogen into angiotensin I. Angiotensinogen is synthesized by the liver and is inactive. As angiotensin I traverses the lungs, ACE (angiotensin-converting-enzyme) converts the angiotensin I into angiotensin II. ACE is found on the surface of vascular endothelial cells, primarily those of the lungs.
Angiotensin II is a potent vasoconstrictor. It will cause vasoconstriction by increasing peripheral resistance. In addition to elevating blood pressure through direct vasoconstriction, Angiotensin II also spurs the adrenal gland to release aldosterone, which causes the renal tubules to increase the reabsorption of sodium into the blood. So sodium levels in the blood increase, which increases the osmotic potential of the blood and attract more water into the vessels. In this process, potassium excretion synchronously increases to keep electrolyte balance. Moreover, the pituitary gland will release ADH (antidiuretic hormone), which will cause the kidneys to keep water. The more water flux into the plasma makes blood volumes bigger. The increased volumes will further increase venous return, resulting in blood pressure increase.
Conversely, the systemic blood pressure increases, the pressure in the afferent arteriole will also increase. The juxtaglomerular cells will detect the alteration and reduce renin secretion. As less renin enters the blood, the activation of angeotensionogen will reduce, remaining more angeotensionogen in an inactive form. The renin-angiotensin pathway allows the kidneys to regulate their blood flow to an extent, a process known as autoregulation.
However, if the renin-angiotensin system is abnormally or excessively active, blood pressure will be too high, which may lead to hypertension. Many drugs block different steps in this system to lower blood pressure. These drugs can control high blood pressure, kidney failure, heart failure, and baleful effects of diabetes.