[1] Mills, Kingston HG. "IL-17 and IL-17-producing cells in protection versus pathology." Nature Reviews Immunology 23.1 (2023): 38-54.
[2] Baker, Kevin James, Elizabeth Brint, and Aileen Houston. "Transcriptomic and functional analyses reveal a tumour-promoting role for the IL-36 receptor in colon cancer and crosstalk between IL-36 signalling and the IL-17/IL-23 axis." British Journal of Cancer 128.5 (2023): 735-747.
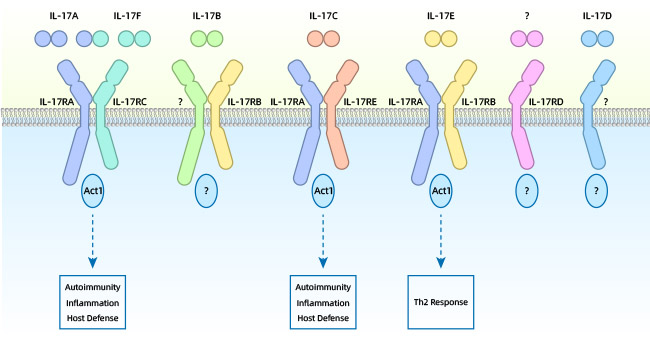
[3] McGeachy, Mandy J., Daniel J. Cua, and Sarah L. Gaffen. "The IL-17 family of cytokines in health and disease. "Immunity 50.4 (2019): 892-906.
[4] Brevi, Arianna, et al. "Much more than IL-17A: cytokines of the IL-17 family between microbiota and cancer." Frontiers in immunology 11 (2020): 565470.
[5] Watad, Abdulla, et al. "Normal human enthesis harbours conventional CD4+ and CD8+ T cells with regulatory features and inducible IL-17A and TNF expression." Annals of the rheumatic diseases 79.8 (2020): 1044-1054.
[6] Le, Thai Van Thanh, et al. "Increased circulatory interleukin-17A levels in patients with progressive and leukotrichial vitiligo. "Dermatology research and practice 2021 (2021).
[7] Brevi, Arianna, et al. "Much more than IL-17A: cytokines of the IL-17 family between microbiota and cancer." Frontiers in immunology 11 (2020): 565470.
[8] Di Padova, Franco, and Jose Carballido. "IL-17A as a Therapeutic Target for Autoimmune Diseases. "IL-17, IL-22 and Their Producing Cells: Role in Inflammation and Autoimmunity (2013): 333-347.
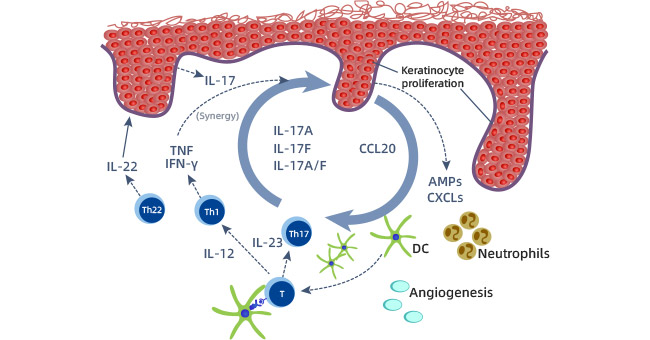
[9] Martin, David A., et al. "The emerging role of IL-17 in the pathogenesis of psoriasis: preclinical and clinical findings." Journal of Investigative Dermatology 133.1 (2013): 17-26.
[10] Nakajima, Saeko, et al. "IL-17A as an inducer for Th2 immune responses in murine atopic dermatitis models." journal of Investigative Dermatology 134.8 ( 2014): 2122-2130.
[11] Brembilla, Nicolo Costantino, Luisa Senra, and Wolf-Henning Boehncke. "The IL-17 family of cytokines in psoriasis: IL-17A and beyond. "Frontiers in immunology 9 (2018): 1682.
[12] Tan, Haitao, Shan Huang, and Tingrui Wang. "Clinical significance of peripheral blood Th1 and Th17 cell content and serum il-35 and il-17 expression in patients with ankylosing spondylitis." Evidence-Based Complementary and Alternative Medicine 2022 (2022).
[13] Bhardwaj, Supriya, et al. "Role of IL-17A receptor blocking in melanocyte survival: a strategic intervention against vitiligo." Experimental Dermatology 28.6 (2019): 682-689.
[14] Sirikanjanapong, Sasis, et al. "Collision tumor of primary laryngeal mucosal melanoma and invasive squamous cell carcinoma with IL-17A and CD70 gene over-expression." Head and neck pathology 4 (2010): 295-299.
[15] Chen, Chen, and Feng-Hou Gao. "Th17 cells paradoxical roles in melanoma and potential application in immunotherapy. "Frontiers in Immunology 10 (2019) : 187.
[16] Ganzetti, Giulia, et al. "IL-17, IL-23, and p73 expression in cutaneous melanoma: a pilot study." Melanoma Research 25.3 (2015): 232-238.
[17] Liu, Chao, et al. "Blocking IL-17A enhances tumor response to anti-PD-1 immunotherapy in microsatellite stable colorectal cancer." journal for immunotherapy of cancer 9.1 (2021).
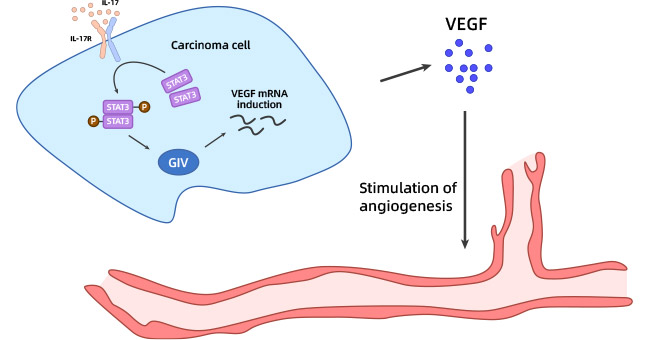
[18] Yu, Chunyan, et al. "IL-17A promotes fatty acid uptake through the IL-17A/IL-17RA/p-STAT3/FABP4 axis to fuel ovarian cancer growth in an adipocyte- rich microenvironment." Cancer Immunology, Immunotherapy 69 (2020): 115-126.
[19] von Stebut, Esther, et al. "IL-17A in psoriasis and beyond: cardiovascular and metabolic implications." Frontiers in immunology 10 (2020): 3096.
[20] Dubash, Sayam, et al. "The advent of IL-17A blockade in ankylosing spondylitis: secukinumab, ixekizumab and beyond." expert review of clinical immunology 15.2 (2019): 123-134.
[21] Montúfar-Robles, Isela, et al. "IL-17A haplotype confers susceptibility to systemic lupus erythematosus but not to rheumatoid arthritis in Mexican patients." International Journal of Rheumatic Diseases 22.3 (2019): 473-479.
[22] Chen, Chen, and Feng-Hou Gao. "Th17 cells paradoxical roles in melanoma and potential application in immunotherapy. "Frontiers in Immunology 10 (2019) : 187.
[23] Wei, Calvin, et al. "Primary mucosal melanoma arising from the eustachian tube with CTLA-4, IL-17A, IL-17C, and IL-17E upregulation. "Ear, Nose & Throat Journal 92.1 (2013): 36-40.
[24] Ghahartars, Mehdi, et al. "Investigation of IL-17A serum levels in patients with nonmelanoma skin cancer." Dermatology Research and Practice 2021 ( 2021): 1-5.
[25] Ganzetti, Giulia, et al. "IL-17, IL-23, and p73 expression in cutaneous melanoma: a pilot study." Melanoma Research 25.3 (2015): 232-238.
[26] Li Yanshuang, et al. "In vivo anti-tumor mechanism of mouse colon cancer cells transfected with IL-17 gene." Chinese Journal of Immunology 31.5 (2015). 643-649.
[27] Wang, Dan, et al. "Serum CCL20 combined with IL-17A as early diagnostic and prognostic biomarkers for human colorectal cancer." journal of translational medicine 17 (2019): 1-11.
[28] Yu, Chunyan, et al. "IL-17A promotes fatty acid uptake through the IL-17A/IL-17RA/p-STAT3/FABP4 axis to fuel ovarian cancer growth in an adipocyte- rich microenvironment." Cancer Immunology, Immunotherapy 69 (2020): 115-126.
[29] Li, Xiaojing, et al. "Celastrol strongly inhibits proliferation, migration and cancer stem cell properties through suppression of Pin1 in ovarian cancer cells." European Journal of Pharmacology 842 (2019): 146-156.

-SDS.jpg)
-AC1.jpg)



Comments
Leave a Comment