Yellow fever virus
Yellow fever virus (YFV) is an RNA virus that belongs to the genus Flavivirus. Over 100 species comprise the genus Flavivirus, which includes other notable human pathogens, such as dengue virus (DENV), Japanese encephalitis virus (JEV), Zika virus (ZIKV), West Nile virus (WNV), Kyasanur Forest disease virus, and tick-borne encephalitis virus.
The yellow fever virus originated in Africa and circulated between Aedes aegypti mosquito and monkeys in the rain forests of Africa for thousands of years [1]. It is a potential deadly mosquito-borne flavivirus, which can be transmitted to humans through the bites of certain Aedes or Haemagogus species of mosquitoes. Today, yellow fever is on the rise. In 2013 the World Health Organization reported 127,000 severe cases and 45,000 deaths. It is estimated that 90% of yellow fever infections occur in Africa, with large portions of South America also considered at risk.
Read on to learn more about YFV, including structure, the important proteins, infection mechanisms, infection symptoms, transmission, diagnosis and treatment.
The Structure and Important Proteins
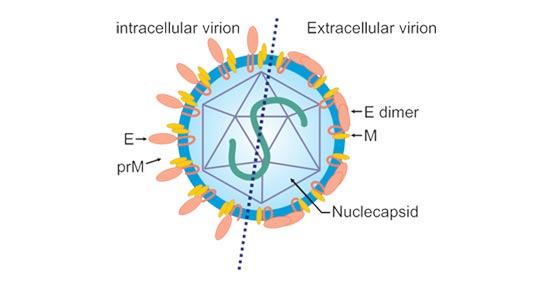
Mature YFV virion is an icosahedral particle about 40 nm in diameter. Like other flaviviruses, YFV contains a small glycoprotein-containing lipid envelope surrounding a nucleocapsid which encloses one viral RNA. The envelope of virus is inlaid with two virally encoded proteins: envelope (E) protein and membrane (M) protein. The E glycoprotein is the major component of the virion surface and is responsible for the receptor-mediated endocytic fusion and subsequent cell entry, as well as direct viral assembly & budding, and immunogenicity.
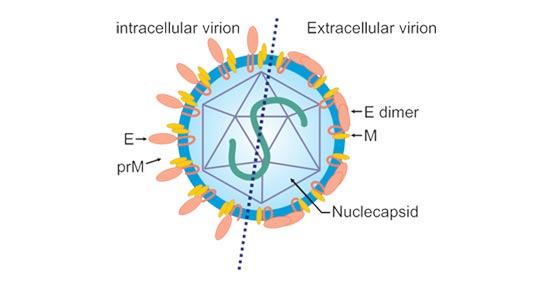
Figure 1. The immature (intracellular) and mature (extracellular) infectious virion.
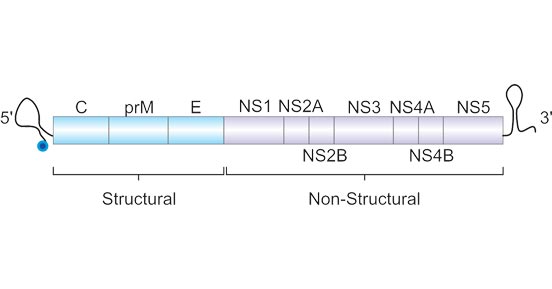
The viral genome is a single positive-stranded, infectious RNA molecule, about 11 kb in length. This 11-kb molecule is made up of 5′- and 3′-untranslated regions (UTRs), between which lie a single open reading frame (ORF) encoding three structural proteins (capsid [C], premembrane [PrM], and envelope [E]) and seven nonstructural (NS) proteins (NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5).
Figure 2. The yellow fever virus genome.
Related Proteins
Yellow Fever Outbreak Event
The first recorded yellow fever epidemic occurred in the Yucatan Peninsula of Mexico in 1648 [1]. For the next 200 years, yellow fever was widely epidemic in tropical America, the North American coastal cities, and Europe [2]. Since YF vaccine was developed and mass vaccination coverage was carried out, the number of infected cases were dramatically declined. Recently, there have been deadly outbreaks of YFV disease in Angola (2016), the Democratic Republic of the Congo (DRC) (2016), and Brazil (2017) [3].
If yellow fever virus is introduced into an immunodeficient population with human blood loving vectors, coupled with the absence of clear management guidelines and appropriate precautions, there is a great possibility of yellow fever outbreak in this area.
Table: Major historical outbreak events of the yellow fever.
| Year |
County or Territory |
Suspected YF cases |
Deaths from suspected cases |
Confirmed YF cases |
Deaths from confirmed cases |
| 1945-1971 |
Nigeria |
|
|
200000 per year |
30000 per year |
| 2005–2016 |
Sudan |
|
|
1,508 |
368 |
| 2016 |
Angola |
4347 |
377 |
884 |
121 |
| 2016 |
Democratic Republic of the Congo (DRC) |
2987 |
121 |
78 |
16 |
| 2016-2018 |
Brazil |
|
|
2050 |
681 |
Transmission
The yellow fever virus is mainly transmitted to people through the bite of infected Aedes or haemoarchaea mosquitoes [4]. Mosquitoes acquire the virus by feeding on the infected human or non-human primates and then spread it to other human or non-human primates. Infected people are infectious to mosquitoes (known as "viremic") shortly before the fever and within 5 days after the onset of the disease.
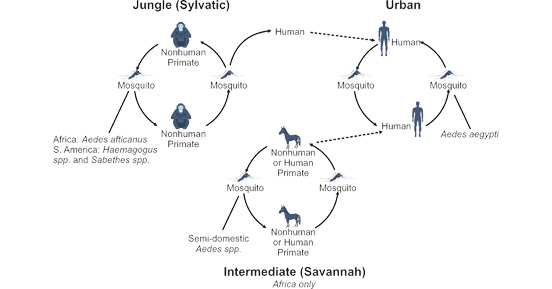
There are three transmission routes of yellow fever virus, including the jungle (sylvatic) cycle, the intermediate (savannah) cycle, the urban cycle [5][6]. They are known as yellow fever virus transmission cycles. In the jungle (sylvatic) cycle, mosquitoes of the forest canopy disperse virus to non-human primates (such as monkeys) and secondarily to humans entering the jungle. The intermediate (savannah) cycle in which virus enters rural towns and villages bordering jungle areas in Africa. In this cycle, the virus can be propagated from monkey to human or from human to human via mosquitoes. Within urban areas, YFV can rapidly spread due to mosquito–human–mosquito transmission (mainly refers to Aedes aegypti mosquitoes).
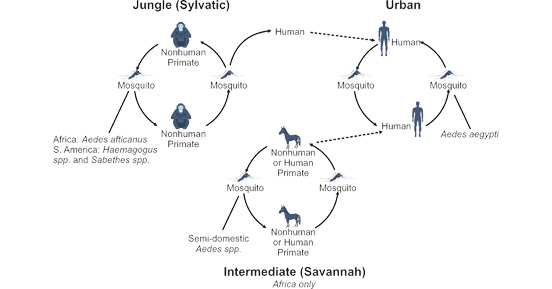
Figure 3. Three transmission routes of yellow fever virus
References
[1] Carter HR. Yellow fever: an epidemiological and historical study of its place of origin. Williams & Wilkins; Baltimore (MD): 1931.
[2] Strode GK, ed, Bugher JC, ed, et al. Yellow Fever. New York, NY: McGraw-Hill Book Co; 1951.
[3] World Health Organization. Yellow fever. http://www.who.int/topics/yellow_fever/en/. Accessed April 26, 2017.
[4] Bryan CS, Moss SW, Kahn RJ. Yellow fever in the Americas. Infect Dis Clin North Am. 2004;18(2):275-29215145381.
[5] Centers for Disease Control and Prevention. Yellow fever. https://www.cdc.gov/yellowfever/index.html. Accessed April 26, 2017.
[6] Monath TP, Gershman M, Staples JE, Barrett A. Yellow fever vaccine In: Plotkin SA, Orenstein WA, Offit PA, eds. Vaccines. Philadelphia, PA: Saunders; 2012:870–968.